Taking 100mg of Zoloft while breastfeeding requires careful consideration. Consult your doctor immediately; they’ll assess your specific situation and weigh the benefits of medication against potential risks to your baby. This personalized assessment is paramount.
Low levels of sertraline (the active ingredient in Zoloft) can transfer into breast milk. Research suggests that at 100mg, these levels are generally considered low and may not significantly impact the infant. However, every individual reacts differently, and monitoring your baby for potential side effects is crucial.
Potential side effects in infants exposed to Zoloft through breast milk are rare but can include sleepiness, irritability, and feeding difficulties. Closely observe your baby’s behavior and report any concerning changes to your physician. Regular checkups are recommended to ensure your baby’s wellbeing.
Remember, this information is for guidance only and doesn’t replace professional medical advice. Always discuss your medication with your healthcare provider before making any changes to your treatment plan, particularly when breastfeeding. They can provide accurate, personalized recommendations tailored to your needs and circumstances.
- 100 mg of Zoloft While Breastfeeding: A Detailed Guide
- Monitoring Your Baby
- Zoloft and Breast Milk
- Alternative Treatment Options
- Dosage Adjustments
- Blood Levels
- Long-Term Considerations
- Zoloft and Breast Milk Transfer: What We Know
- Factors Affecting Transfer
- Monitoring Your Baby
- Recommendations
- Data Summary
- Seeking Professional Guidance
- Dosage Considerations for Breastfeeding Mothers on Zoloft
- Monitoring Baby’s Health
- Adjusting Dosage
- Potential Risks of Zoloft Exposure for Infants
- Rare but Serious Risks
- Monitoring and Recommendations
- Neonatal Withdrawal
- Monitoring Infant for Side Effects
- Alternatives to Zoloft During Breastfeeding
- Consulting Your Doctor: Importance of Personalized Advice
- Weighing the Risks and Benefits: A Personal Decision
- Strategies for Minimizing Infant Exposure
- Supporting Mothers on Zoloft While Breastfeeding
100 mg of Zoloft While Breastfeeding: A Detailed Guide
Consult your doctor immediately before making any decisions about taking Zoloft while breastfeeding. They can assess your individual needs and risks, considering your mental health and your baby’s well-being. A low dose, like 100mg, may be manageable, but careful monitoring is crucial.
Monitoring Your Baby
Regular check-ups with your pediatrician are recommended. They will observe your baby’s growth, development, and feeding patterns. Any unusual symptoms should be reported immediately. Watch for drowsiness, poor feeding, or irritability in your baby.
Zoloft and Breast Milk
Sertraline (Zoloft’s active ingredient) does transfer into breast milk, though the amount is generally low. However, the amount transferred can vary depending on factors like your metabolism and dosage. This is why close monitoring is necessary. Your doctor can help you weigh the benefits of treatment against potential risks to your baby.
Alternative Treatment Options
Discuss non-pharmacological approaches with your doctor if possible. Therapy, lifestyle changes, and support groups can be beneficial in managing postpartum depression or anxiety. If medication is necessary, they may suggest alternative antidepressants with lower levels of transfer into breast milk.
Dosage Adjustments
Your doctor may recommend starting at a lower dose and gradually increasing it, if needed. This allows for careful observation of both your symptoms and your baby’s reaction. Adjustments to your dosage will be based on both your needs and your baby’s response.
Blood Levels
In some cases, your doctor may suggest monitoring sertraline levels in your blood and your baby’s blood (if necessary) to determine the optimal dosage for you and manage potential side effects. This provides a precise understanding of how the medication affects both of you.
Long-Term Considerations
Long-term breastfeeding while on Zoloft requires ongoing vigilance and communication with your healthcare team. Regular check-ups are essential to ensure both your health and your baby’s well-being are consistently monitored. Remember, open communication with your medical professionals is key.
Zoloft and Breast Milk Transfer: What We Know
Sertraline (Zoloft) does transfer into breast milk. Studies show approximately 1% of the maternal dose reaches the infant via breast milk. This translates to a very low level, generally considered safe for most infants.
Factors Affecting Transfer
The amount of sertraline transferred depends on several factors, including the mother’s dosage, metabolism, and the infant’s age and weight. Higher maternal doses may result in slightly higher concentrations in breast milk, but even at higher doses, the levels remain relatively low.
Monitoring Your Baby
Closely observe your baby for any unusual symptoms after initiating or adjusting your Zoloft dosage. While rare, potential side effects in infants can include drowsiness, irritability, or feeding difficulties. Consult your pediatrician if you notice any changes in your baby’s behavior or health.
Recommendations
Open communication with your healthcare provider is key. They can help you weigh the benefits of Zoloft for your mental health against any potential risks to your baby. Individualized recommendations are crucial, as each mother-infant pair is unique.
Data Summary
| Factor | Impact on Sertraline Transfer |
|---|---|
| Maternal Dose | Higher doses correlate with slightly higher levels in breast milk, but still low overall. |
| Infant Age/Weight | Smaller infants may be slightly more susceptible to any effects. |
| Maternal Metabolism | Individual metabolism influences how much sertraline enters the milk. |
Seeking Professional Guidance
Remember, this information is for general knowledge and should not replace advice from your doctor or other qualified healthcare professional. They can provide personalized guidance based on your specific situation and thoroughly assess your individual needs.
Dosage Considerations for Breastfeeding Mothers on Zoloft
The lowest effective dose of Zoloft is generally recommended for breastfeeding mothers. This often starts at 25 mg daily, gradually increasing as needed under close medical supervision. Individual needs vary greatly, so your doctor will personalize your treatment plan based on your symptoms and response to medication. Regular blood tests might monitor medication levels in both you and your baby, ensuring safety and efficacy. Always communicate any changes in your health or your baby’s well-being to your physician immediately.
Monitoring Baby’s Health
While Zoloft levels in breast milk are generally low, your doctor will likely recommend close observation of your baby for any potential side effects. This includes monitoring feeding patterns, sleep, and overall development. Early detection of any issues allows for prompt adjustments to your treatment plan. Open communication with your pediatrician is crucial to ensure your baby’s health and well-being.
Adjusting Dosage
Dosage adjustments should only be made by your doctor. Never alter your medication without consulting them. They can guide you through the process of adjusting the dose safely and effectively, minimizing potential risks to both you and your baby. This might involve gradually increasing or decreasing the dose based on your needs and your baby’s response.
Potential Risks of Zoloft Exposure for Infants
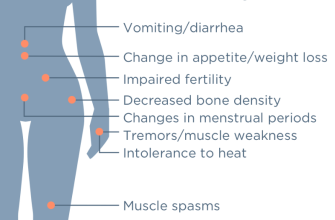
While Zoloft (sertraline) is generally considered safe during breastfeeding, infant exposure carries potential risks. The amount of sertraline transferred to the infant through breast milk is usually low, but it can still cause effects. Studies show that infants exposed to sertraline may experience irritability, feeding difficulties, and sleep disturbances. These symptoms are usually mild and resolve upon cessation of maternal Zoloft use.
Rare but Serious Risks
Less commonly, infants may exhibit other symptoms including jitteriness, tremors, and respiratory problems. These are generally less frequent and tend to be dose-related; meaning, higher maternal doses are linked to a slightly increased risk. It’s important to carefully monitor the infant for any unusual behaviors or health concerns.
Monitoring and Recommendations
Regular monitoring by your pediatrician is recommended for infants exposed to sertraline. This involves close observation for any of the mentioned symptoms. Consider keeping a detailed record of your infant’s feeding, sleep patterns, and any unusual behaviors. This information is invaluable for your pediatrician’s assessment.
Discuss all medications with your healthcare provider, including your obstetrician and pediatrician, before, during, and after breastfeeding to optimize both your well-being and your infant’s safety. They can help weigh the benefits of continuing Zoloft against the potential risks to your baby. This includes considering alternative treatment options for postpartum depression or anxiety. A collaborative approach is crucial for making informed decisions.
Neonatal Withdrawal
If the infant exhibits symptoms of withdrawal after birth, a pediatrician may recommend a gradual reduction of maternal sertraline dosage to minimize the occurrence of withdrawal symptoms in the infant.
Monitoring Infant for Side Effects
Closely observe your baby for any unusual changes. Weigh your baby regularly to monitor growth.
Note any changes in feeding patterns, such as decreased appetite or difficulty latching. Pay close attention to sleep patterns – increased drowsiness or irritability could be significant.
Track bowel movements. Changes in frequency or consistency warrant attention. Monitor your baby’s temperature frequently.
Report any symptoms, including unusual skin reactions, excessive crying, or lethargy, to your pediatrician immediately. Document all observations meticulously.
Your doctor may recommend additional monitoring, such as blood tests, to assess your baby’s overall health. Maintain open communication with your healthcare provider; they are your best resource.
Alternatives to Zoloft During Breastfeeding
Consider consulting your doctor about other antidepressants. Sertraline (Zoloft) does pass into breast milk, but many others do as well, at varying levels. Your doctor can assess your specific needs and the risks versus benefits of different medications. They can help you choose an antidepressant with a lower level of transfer into breast milk or one deemed safer for breastfeeding mothers.
Non-pharmacological approaches also merit exploration. Cognitive Behavioral Therapy (CBT) and other forms of therapy can be highly effective in managing postpartum depression and anxiety. These methods don’t involve medication and are safe for both you and your baby. Your physician can help you find a qualified therapist.
Lifestyle adjustments play a crucial role. Prioritize adequate sleep, a balanced diet, and regular exercise. A strong support system, including family and friends, can make a significant difference. Joining a support group for new mothers can provide invaluable emotional support and practical advice.
Remember, the best alternative for you depends on individual circumstances. Open communication with your healthcare provider ensures you receive tailored advice and support to manage your mental health while breastfeeding.
Consulting Your Doctor: Importance of Personalized Advice
Always discuss your medication with your doctor before breastfeeding. They can assess your individual circumstances and provide tailored advice.
Factors your doctor will consider include:
- Your baby’s age and weight
- Your medical history
- Your overall health
- The amount of Zoloft you’re taking
- Any potential side effects in you or your baby
Your doctor might recommend:
- Adjusting your Zoloft dosage.
- Monitoring your baby for any adverse reactions.
- Regular checkups for both you and your baby.
- Alternative medication options, if needed.
- Closely tracking your baby’s growth and development.
Don’t hesitate to ask your doctor questions. Clear communication ensures you both understand the risks and benefits. This proactive approach protects your health and your baby’s well-being.
Regular follow-up appointments are vital. This allows your doctor to make adjustments as needed and ensures the best possible outcome for both of you.
Weighing the Risks and Benefits: A Personal Decision
Consult your doctor. They can provide personalized advice based on your specific circumstances and health history. This includes considering your baby’s age and weight, your dosage of Zoloft, and your overall health. Open communication with your healthcare provider is key.
Research Zoloft’s effects on breast milk. Understand the potential for your baby to ingest trace amounts of the medication. Look for reliable sources, such as medical journals and government health websites. Your doctor can help you find and interpret this information.
Assess your mental health. Untreated postpartum depression or anxiety can negatively impact both you and your baby. Weigh the potential risks of untreated mental illness against the possible risks of Zoloft exposure. This requires honest self-assessment and a discussion with your doctor.
Explore alternative treatments. If you’re concerned about Zoloft while breastfeeding, discuss other treatment options for your condition with your doctor. These could include therapy, lifestyle changes, or different medications. This is a collaborative process; your doctor will help you find what works best.
Monitor your baby. If you choose to continue breastfeeding while taking Zoloft, closely monitor your baby for any unusual symptoms. This could include changes in feeding patterns, sleep, or behavior. Report any concerns immediately to your healthcare provider.
Remember, the decision of whether or not to take Zoloft while breastfeeding is deeply personal. Prioritize open communication with your doctor. Together, you can make an informed choice that best suits your needs and your baby’s well-being. Trust your instincts and advocate for your health.
Strategies for Minimizing Infant Exposure
Choose the lowest effective dose of Zoloft. Work closely with your doctor to find the minimum dose that manages your symptoms effectively. Reducing your dose, if possible and medically sound, directly reduces the amount transferred to your baby through breast milk.
Time your medication strategically. Take Zoloft at a time when your baby will likely be sleeping or shortly before nursing, allowing for some drug metabolism before breastfeeding.
Pump and discard. Pump breast milk before you take your medication. This removes a portion of milk that contains the higher concentration of medication from the previous dose.
- Consider pumping and discarding milk for several hours after medication administration. Consult your healthcare professional about the appropriate duration.
Monitor your baby. Watch your baby carefully for any unusual side effects, such as drowsiness, poor feeding, or changes in bowel movements. If you notice any changes, contact your pediatrician immediately.
- Keep a detailed record of your medication schedule and your baby’s feeding and sleeping patterns.
- Note any changes in your baby’s behavior or health that might correlate to medication exposure.
Seek expert advice. Regularly consult with your doctor and a lactation consultant who can provide personalized guidance tailored to your specific situation and medication dosage.
Explore alternative treatments. Discuss non-pharmacological options with your physician, such as therapy, lifestyle adjustments, or other suitable interventions. This may allow a reduction or even elimination of Zoloft. Remember to discuss all treatment options with your doctor before making any changes.
Supporting Mothers on Zoloft While Breastfeeding
Maintain open communication with your doctor and a lactation consultant. Regular check-ups monitor your baby’s health and your medication dosage. This collaborative approach ensures both your well-being and your baby’s.
Choose a breastfeeding-friendly positioning technique for optimal milk transfer. This often minimizes baby’s exposure to medication. Ask your lactation consultant for personalized guidance.
Monitor your baby for any unusual symptoms, like excessive sleepiness or poor feeding. Report any concerns immediately to your pediatrician and your prescribing physician. Early intervention is vital.
Consider pumping and discarding breast milk immediately after taking Zoloft. This minimizes the medication’s concentration in milk your baby consumes. Your doctor can advise on how long to discard.
Prioritize self-care. Adequate rest, a balanced diet, and stress management techniques support both mental and physical health. This contributes to successful breastfeeding and overall well-being.
Explore support groups for breastfeeding mothers and those taking antidepressants. Connecting with others facing similar challenges provides invaluable emotional support and practical advice. Online forums and local chapters are great resources.
Remember, many mothers successfully breastfeed while managing their mental health with medication like Zoloft. With proper medical guidance and support, you can too.