Prednisone, a synthetic glucocorticoid, significantly impacts your adrenal glands. Understanding this interaction is key to managing your treatment effectively. Specifically, long-term prednisone use can suppress your adrenal glands’ natural cortisol production. This means your body becomes reliant on the medication.
Your adrenal glands produce cortisol, vital for managing stress, inflammation, and blood sugar. Prednisone mimics cortisol’s actions, but prolonged use tricks your body into thinking it doesn’t need to produce its own. This suppression can lead to adrenal insufficiency upon sudden cessation of prednisone, resulting in fatigue, nausea, and even life-threatening complications.
Gradual tapering of prednisone dosage under medical supervision is paramount. Your doctor will carefully reduce your dose over weeks or months to allow your adrenal glands to resume their normal function. Regular monitoring of cortisol levels helps determine the appropriate tapering schedule and prevents abrupt withdrawal symptoms.
Always discuss potential side effects and any concerns with your healthcare provider. They can provide personalized advice based on your individual health status and prednisone regimen. Open communication is crucial for safe and successful management of your treatment.
- Adrenal Glands Function and Prednisone
- Adrenal Gland Function
- Prednisone’s Impact
- Managing Prednisone Use
- Dosage and Tapering Schedule (Example)
- Long-Term Effects
- Understanding the Adrenal Glands’ Role in the Body
- Cortisol’s Impact on the Body
- Aldosterone and Fluid Balance
- Cortisol: The Key Hormone Affected by Prednisone
- How Prednisone Mimics Cortisol Production
- Mechanism of Action
- Specific Effects Mimicking Cortisol
- Important Note
- Short-Term vs. Long-Term Prednisone Use: Impacts on Adrenal Function
- Adrenal Suppression with Long-Term Use
- Managing Adrenal Function During and After Prednisone Treatment
- Individual Variation
- Adrenal Suppression: Symptoms and Risks
- Recognizing Adrenal Suppression
- Risks of Adrenal Suppression
- Managing Adrenal Suppression
- Tapering Off Prednisone: A Crucial Step for Adrenal Recovery
- Monitoring Your Body’s Response
- Managing Potential Side Effects
- The Importance of Patience
- Maintaining a Healthy Lifestyle
- Monitoring Adrenal Function During and After Prednisone Treatment
- Potential Complications and Management Strategies
Adrenal Glands Function and Prednisone
Prednisone, a synthetic glucocorticoid, mimics the cortisol your adrenal glands naturally produce. Understanding your adrenal glands’ role is key to understanding how prednisone works and its potential effects.
Adrenal Gland Function
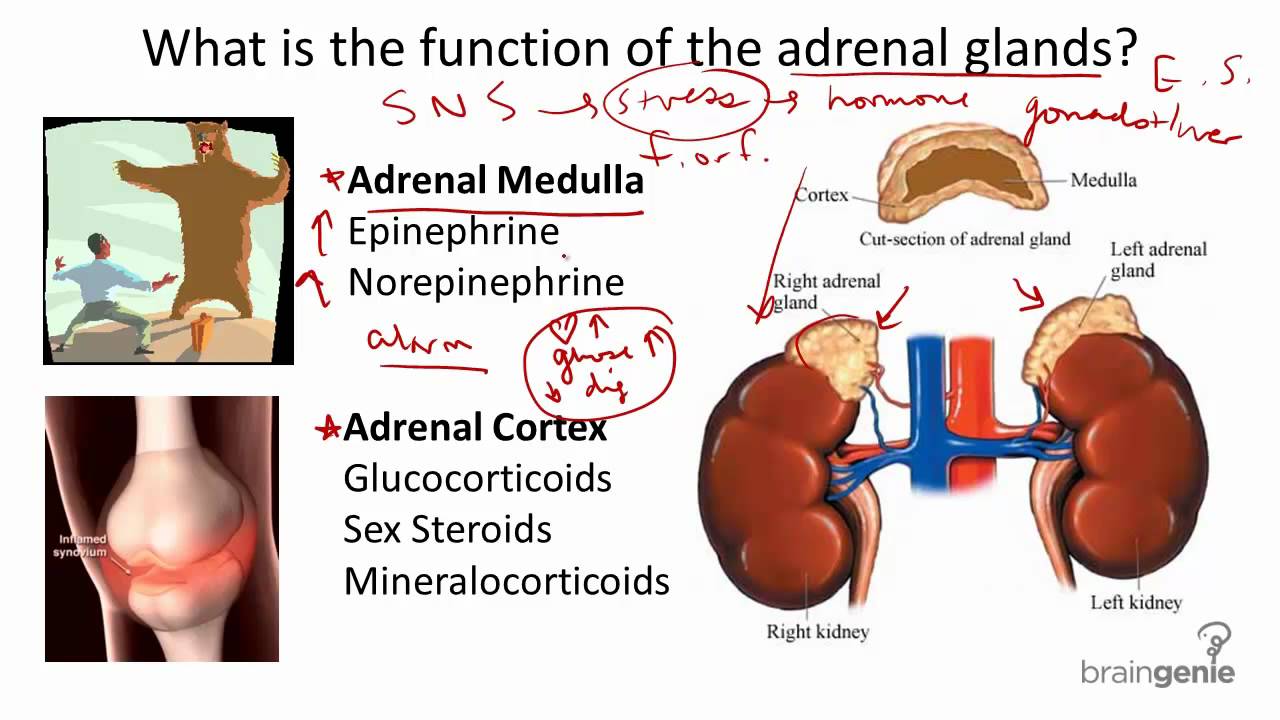
Your adrenal glands, located atop your kidneys, are vital for managing stress, regulating blood sugar, and supporting your immune system. They produce several hormones, including cortisol, aldosterone, and androgens. Cortisol, the primary glucocorticoid, influences metabolism, blood pressure, and inflammation. Its production follows a circadian rhythm, peaking in the morning and decreasing throughout the day.
Prednisone’s Impact
Prednisone supplements or replaces your body’s natural cortisol. High doses or prolonged use suppress your adrenal glands’ ability to produce cortisol. This suppression can lead to adrenal insufficiency upon cessation of prednisone, manifesting as fatigue, nausea, and low blood pressure. This is why prednisone is usually tapered gradually, allowing your adrenal glands to resume normal function.
Managing Prednisone Use
Close monitoring is crucial. Your doctor will adjust your dosage based on your response and needs. Potential side effects include increased blood sugar, weight gain, mood changes, and increased risk of infections. Dietary changes, like monitoring sugar intake, may be recommended to manage side effects. Open communication with your doctor regarding any concerns is paramount.
Dosage and Tapering Schedule (Example)
| Day | Prednisone Dose (mg) |
|---|---|
| 1-7 | 40 |
| 8-14 | 30 |
| 15-21 | 20 |
| 22-28 | 10 |
| 29-35 | 5 |
| 36+ | 0 |
Note: This is a sample schedule. Your doctor will create a personalized tapering plan based on your individual needs and health status. Never alter your prednisone dosage without consulting your physician.
Long-Term Effects
Long-term prednisone use carries a greater risk of complications. Regular check-ups with your doctor are essential for monitoring your health and managing potential side effects. They may perform blood tests to assess your adrenal function and overall health.
Understanding the Adrenal Glands’ Role in the Body
Your adrenal glands, small glands perched atop your kidneys, are vital for managing stress and regulating many bodily functions. They produce various hormones, most notably cortisol and aldosterone. Cortisol helps regulate metabolism, blood sugar, blood pressure, and the immune system’s response to inflammation and injury. Aldosterone maintains sodium and potassium balance, directly affecting blood volume and pressure.
Cortisol’s Impact on the Body
Cortisol, often called the “stress hormone,” plays a crucial role in your body’s response to physical and emotional stress. It triggers the release of glucose into the bloodstream, providing immediate energy. It also suppresses inflammation. However, chronically high cortisol levels can negatively affect immune function, bone density, and cardiovascular health. Maintaining a healthy cortisol balance is paramount for overall well-being.
Aldosterone and Fluid Balance
Aldosterone’s primary function is managing fluid balance by influencing how your kidneys handle sodium and potassium. It signals your kidneys to retain sodium and excrete potassium, thereby regulating blood volume and blood pressure. Imbalances in aldosterone can lead to issues such as high blood pressure or low blood pressure, highlighting its importance in maintaining homeostasis.
Understanding how your adrenal glands function provides valuable insights into your overall health and the potential impact of conditions like adrenal insufficiency or Cushing’s syndrome. Consulting a healthcare professional is advisable for any concerns regarding adrenal gland function.
Cortisol: The Key Hormone Affected by Prednisone
Prednisone mimics cortisol, a steroid hormone your adrenal glands naturally produce. This hormone regulates numerous bodily functions, including metabolism, immune response, and blood pressure.
Prednisone’s impact stems from its ability to bind to the same receptors as cortisol, triggering similar cellular responses. High doses suppress your adrenal glands’ natural cortisol production. This suppression is temporary, usually reversing upon discontinuation.
Gradual tapering of prednisone dosage is crucial to allow your adrenal glands to resume their function. Sudden cessation can lead to adrenal insufficiency, characterized by fatigue, nausea, and low blood pressure. Your doctor will guide you on a safe tapering schedule.
While prednisone provides significant therapeutic benefits, long-term use carries risks. These risks include increased blood sugar, bone loss, and increased susceptibility to infections. Regular monitoring of blood pressure, blood sugar, and bone density is necessary during prolonged treatment.
Always discuss any concerns with your physician. They can help manage potential side effects and determine the appropriate dosage and duration of prednisone treatment tailored to your specific needs.
How Prednisone Mimics Cortisol Production
Prednisone, a synthetic glucocorticoid, works by binding to the same receptors as cortisol, your body’s natural stress hormone. This binding triggers a cascade of cellular events, mimicking cortisol’s effects throughout your system.
Mechanism of Action
Cortisol and prednisone bind to glucocorticoid receptors (GRs) located inside cells. This binding alters gene expression, leading to changes in protein production. Specifically, it impacts the production of proteins that regulate:
- Inflammation
- Immune response
- Metabolism of carbohydrates, proteins, and fats
- Blood pressure
The potency of prednisone surpasses that of cortisol, allowing lower doses to achieve significant therapeutic effects. This difference in potency stems from its higher affinity for GRs and a longer half-life, meaning it stays in your system longer.
Specific Effects Mimicking Cortisol
- Anti-inflammatory actions: Prednisone inhibits the production of inflammatory molecules like cytokines, reducing swelling and pain.
- Immunosuppression: It dampens the activity of the immune system, helpful in autoimmune diseases but increasing susceptibility to infections.
- Metabolic effects: Prednisone influences blood sugar levels, often leading to increased blood glucose, mimicking cortisol’s impact on glucose metabolism.
- Fluid balance: Similar to cortisol, it influences sodium and water retention, potentially leading to fluid accumulation.
Important Note
While prednisone effectively mimics cortisol’s actions, it’s crucial to remember it’s not a perfect substitute. Long-term use can lead to significant side effects due to its potent effects on various bodily systems. Always follow your doctor’s instructions for dosage and duration of treatment.
Short-Term vs. Long-Term Prednisone Use: Impacts on Adrenal Function
Prednisone, a synthetic glucocorticoid, mimics cortisol, a hormone your adrenal glands naturally produce. Short-term use (typically less than 3 weeks) usually doesn’t significantly suppress adrenal function. Your body continues producing cortisol, albeit potentially at a slightly reduced rate while taking prednisone. However, extended prednisone use (more than 3 weeks, especially at higher doses) significantly alters this dynamic.
Adrenal Suppression with Long-Term Use
Prolonged prednisone use leads to adrenal suppression. Your adrenal glands become less responsive to the body’s signals to produce cortisol. This happens because prednisone provides an external source of cortisol, effectively “telling” your adrenal glands to slow their production. The degree of suppression depends on the dose and duration of prednisone therapy. Stopping prednisone abruptly after prolonged use can cause adrenal insufficiency, a serious condition where your body lacks sufficient cortisol. This insufficiency manifests as fatigue, weakness, nausea, and low blood pressure.
Managing Adrenal Function During and After Prednisone Treatment
Gradual tapering is crucial when discontinuing long-term prednisone. Your doctor will slowly reduce your dose over weeks or even months, allowing your adrenal glands to gradually resume cortisol production. Regular monitoring of cortisol levels through blood tests aids in safe tapering. During tapering, you might experience symptoms of adrenal insufficiency like fatigue or nausea; these symptoms will likely subside once your adrenal glands regain function. The duration of this recovery varies depending on factors like the dose and duration of prednisone use, but it can take several months.
Individual Variation
Individual responses to prednisone vary greatly. Factors like your overall health, age, and the specific dose and duration of prednisone impact how your adrenal glands respond. Close communication with your healthcare provider is key for personalized treatment and monitoring. They will help you determine the appropriate dosage, duration of therapy, and tapering schedule, minimizing risks and ensuring a smooth recovery.
Adrenal Suppression: Symptoms and Risks
Prolonged prednisone use can suppress your adrenal glands’ natural cortisol production. This means your body makes less of this vital hormone. Recognizing the signs is key.
Recognizing Adrenal Suppression
- Fatigue: Persistent tiredness, even after adequate sleep.
- Muscle weakness: Difficulty performing everyday tasks requiring physical exertion.
- Weight changes: Significant weight gain or loss, often accompanied by changes in body fat distribution.
- Mood swings: Increased irritability, anxiety, or depression.
- Low blood pressure: A reading lower than normal, potentially causing dizziness or fainting.
- Nausea and vomiting: Unexplained episodes of nausea or vomiting.
- Headaches: Frequent or severe headaches.
These symptoms aren’t always indicative of adrenal suppression, but if you experience several, talk to your doctor.
Risks of Adrenal Suppression
Untreated adrenal suppression poses serious health risks.
- Adrenal crisis: A life-threatening condition where your body doesn’t produce enough cortisol. This can trigger severe symptoms like low blood pressure, shock, and loss of consciousness. Immediate medical attention is required.
- Increased infection risk: Cortisol plays a role in the immune system; lower levels increase your susceptibility to infections.
- Osteoporosis: Prolonged cortisol deficiency increases your risk of bone loss and fractures.
- Slow wound healing: Cortisol aids in tissue repair, therefore its deficiency slows down this process.
- Increased risk of blood clots: Low cortisol levels can contribute to problems with blood clotting.
Managing Adrenal Suppression
Your doctor will develop a plan for safely reducing prednisone dosage to minimize the risk of adrenal suppression. This often involves a gradual tapering process. They may also monitor your cortisol levels through blood tests.
Always follow your doctor’s instructions. Open communication about symptoms and concerns is crucial for safe and effective management.
Tapering Off Prednisone: A Crucial Step for Adrenal Recovery
Always work closely with your doctor to create a personalized tapering schedule. A common approach involves gradually reducing your prednisone dose by a small amount at regular intervals, perhaps every few days or weeks, depending on your individual needs and response. This slow decrease allows your adrenal glands to gradually resume their natural cortisol production.
Monitoring Your Body’s Response
Pay close attention to how your body reacts to each dose reduction. Report any new or worsening symptoms to your doctor immediately. These may include fatigue, muscle weakness, nausea, or joint pain. Your doctor may need to adjust the tapering schedule based on your feedback.
Managing Potential Side Effects
Expect some side effects during the tapering process. These are often temporary and manageable. Your doctor can advise on strategies to alleviate discomfort, such as lifestyle adjustments or medication to manage specific symptoms. For example, low doses of hydrocortisone may be prescribed to support your adrenal glands during the transition.
The Importance of Patience
Adrenal recovery takes time. Be patient with the process. Complete recovery can take several months, and a return to baseline cortisol levels may require ongoing monitoring. Regular blood tests will help your doctor track your progress and make necessary adjustments to your treatment plan.
Maintaining a Healthy Lifestyle
Support your adrenal recovery by prioritizing a healthy lifestyle. Eat a balanced diet rich in nutrients, get adequate sleep, manage stress effectively, and engage in regular, moderate exercise. These lifestyle factors significantly contribute to overall well-being and adrenal health.
Monitoring Adrenal Function During and After Prednisone Treatment
Regular monitoring is crucial. Your doctor will likely schedule blood tests to measure cortisol levels. These tests assess your adrenal glands’ ability to produce cortisol, especially during the tapering-off phase of prednisone.
Cortisol levels fluctuate naturally throughout the day, so timing is important. Blood draws are often performed in the morning. Expect multiple tests, especially if you’ve been on prednisone for an extended period.
A common test is the ACTH stimulation test. This involves an injection of ACTH, a hormone that stimulates cortisol production. Blood samples are then taken at intervals to evaluate your adrenal response.
Beyond blood tests, your doctor will monitor you for symptoms of adrenal insufficiency, such as fatigue, weakness, nausea, and low blood pressure. Report any concerning symptoms immediately.
The duration of monitoring depends on several factors including prednisone dosage and duration of treatment. A gradual tapering-off schedule minimizes the risk of adrenal insufficiency. Follow your doctor’s instructions precisely.
Open communication with your doctor is key. Ask questions, express concerns, and ensure you understand the monitoring plan and the meaning of your results. Your proactive participation ensures optimal management of your treatment and recovery.
Potential Complications and Management Strategies
Monitor blood pressure regularly, as prednisone can elevate it. High blood pressure requires careful management, often involving lifestyle changes like diet and exercise, and possibly medication.
Increased blood sugar is another potential side effect. Regular blood glucose checks are crucial, especially for individuals with diabetes or a family history. Dietary adjustments and possibly insulin or other diabetes medications may be necessary.
Prednisone weakens the immune system, increasing susceptibility to infections. Practice good hygiene, avoid crowds during flu season, and promptly report any signs of infection to your doctor. Vaccination is highly recommended.
Osteoporosis is a long-term risk with prolonged prednisone use. Weight-bearing exercise, a calcium-rich diet, and possibly bisphosphonate medication can help mitigate bone loss.
Mood changes, including anxiety and depression, are possible. Open communication with your doctor is vital. They might recommend therapy, medication, or other support strategies.
Cataracts and glaucoma are potential long-term ocular complications. Regular eye exams are necessary to detect and manage these conditions early.
Sudden withdrawal from prednisone can be dangerous. Always taper off the medication gradually under your doctor’s supervision to minimize withdrawal symptoms.
Discuss any concerns or side effects with your physician immediately. They can adjust your dosage, prescribe additional medication, or recommend other management strategies to minimize risks and improve your quality of life.