No, Plavix (clopidogrel) doesn’t directly lower blood pressure. Its primary function is to prevent blood clots, making it crucial for individuals with a history of heart attack, stroke, or peripheral artery disease.
However, reducing blood clot risk can indirectly influence blood pressure in some patients. For example, by preventing clots that might restrict blood flow, Plavix may contribute to improved circulation and thus slightly lower blood pressure in certain cases. This effect is usually subtle and not the drug’s intended action.
It’s vital to remember that Plavix should only be used as prescribed by a doctor. If you’re concerned about your blood pressure, discuss it directly with your physician. They can assess your individual needs and recommend appropriate medications or lifestyle changes to effectively manage your blood pressure. Regular monitoring is key for effective blood pressure control.
- Can Plavix Lower Blood Pressure?
- Why the Confusion?
- What to do if you have high blood pressure?
- Plavix’s Primary Function: Blood Clot Prevention
- How Plavix Prevents Blood Clots
- Understanding Platelet Inhibition
- Important Considerations
- Plavix and Hypertension: A Lack of Direct Impact
- Understanding the Difference
- Managing Both Conditions
- Consult Your Doctor
- Indirect Effects on Blood Pressure: Potential Interactions with Other Medications
- Interactions Affecting Blood Pressure
- Managing Potential Interactions
- Specific Recommendations
- Further Information
- Cases Where Blood Pressure Might Be Affected: Specific Patient Conditions
- Monitoring Blood Pressure While on Plavix: Importance of Regular Checkups
- Alternative Medications for Blood Pressure Management: When Plavix Isn’t Enough
- Consult Your Doctor: Personalized Advice for Your Health
- Understanding Your Individual Needs
- Making Informed Decisions
- Monitoring and Follow-Up
- Lifestyle Modifications
Can Plavix Lower Blood Pressure?
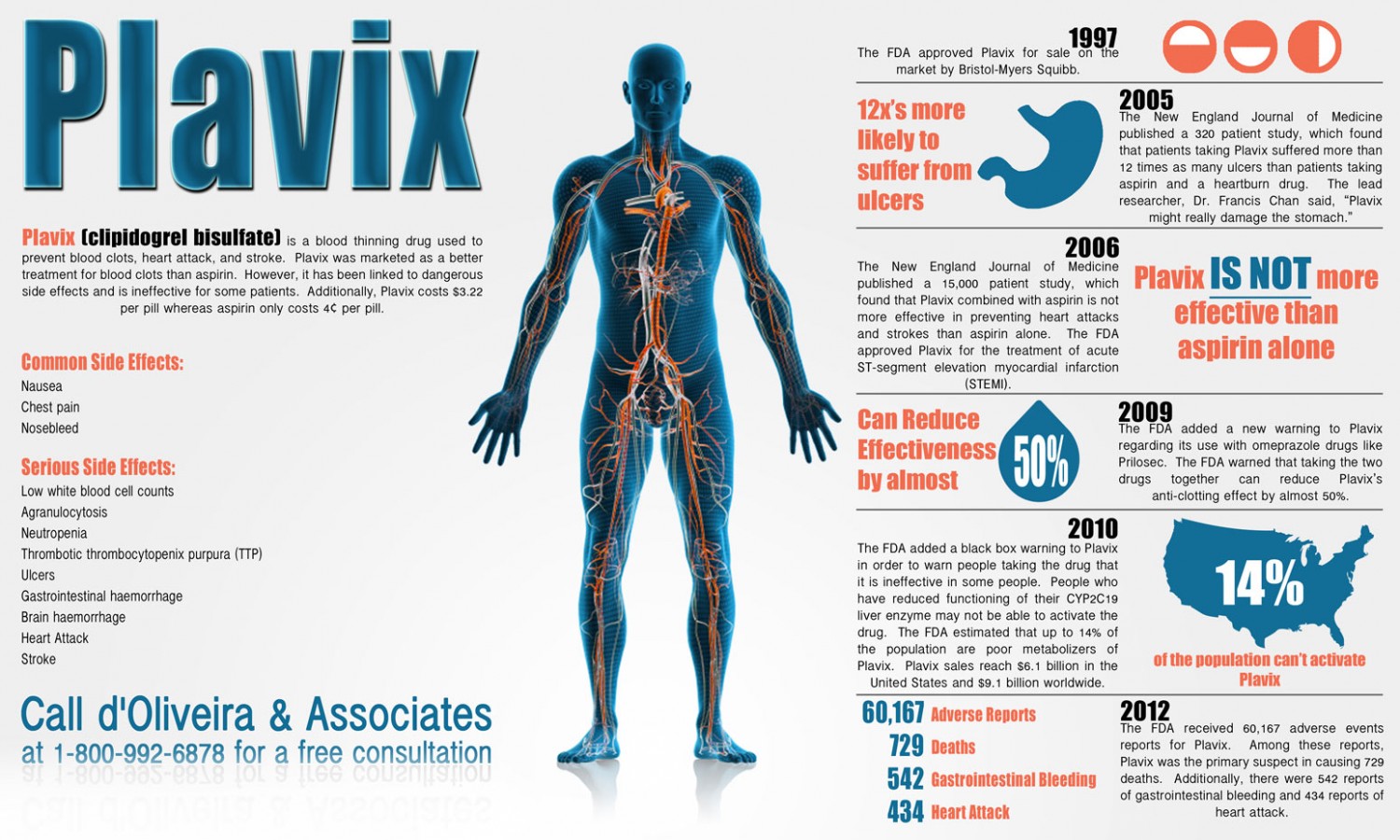
No, Plavix (clopidogrel) doesn’t directly lower blood pressure. It primarily prevents blood clots by inhibiting platelet aggregation. While some studies show a slight, non-significant blood pressure reduction in some patients, this effect isn’t reliable enough to consider Plavix a blood pressure medication.
Why the Confusion?
The confusion arises because conditions like heart disease and stroke, where Plavix is often prescribed, frequently involve hypertension. Treating these underlying conditions, which often include blood pressure management, alongside Plavix, can lead to overall improved cardiovascular health, hence the perception of Plavix contributing to lower blood pressure. However, Plavix’s impact is indirect, resulting from improved overall cardiovascular health, not a direct effect on blood pressure itself.
What to do if you have high blood pressure?
If you have high blood pressure, your doctor will likely prescribe dedicated antihypertensive medications. These medications directly target and regulate blood pressure. Always discuss your medications and treatment plan with your physician. They can determine the best course of action for managing your blood pressure and any other health concerns.
Plavix’s Primary Function: Blood Clot Prevention
Plavix, or clopidogrel, primarily prevents blood clots. It works by inhibiting platelet aggregation, meaning it stops platelets from sticking together and forming clots.
How Plavix Prevents Blood Clots
Platelets are tiny blood cells crucial for wound healing. However, excessive platelet activity can lead to dangerous blood clots blocking arteries, potentially causing heart attacks or strokes. Plavix reduces this risk by making platelets less sticky.
Understanding Platelet Inhibition
Plavix targets a specific receptor on platelets, the P2Y12 receptor. Blocking this receptor prevents the activation of platelets, thus reducing clot formation. This action is vital in preventing cardiovascular events.
| Medication | Mechanism of Action | Clinical Use |
|---|---|---|
| Plavix (Clopidogrel) | Inhibits platelet aggregation by blocking the P2Y12 receptor | Prevention of heart attack, stroke, and other thrombotic events |
Important Considerations
While Plavix is highly effective, it’s crucial to consult your doctor before taking it. They will assess your individual needs and risks, and determine the appropriate dosage and duration of treatment. Remember, this information is for educational purposes and should not replace professional medical advice.
Plavix and Hypertension: A Lack of Direct Impact
Plavix (clopidogrel) doesn’t directly lower blood pressure. Its primary function is to prevent blood clots, not to manage hypertension. Studies haven’t shown a consistent blood pressure-lowering effect from Plavix use.
Understanding the Difference
High blood pressure (hypertension) requires specific medication to control it. Common hypertension drugs include ACE inhibitors, ARBs, beta-blockers, and diuretics. These target the mechanisms that regulate blood pressure.
Managing Both Conditions
Patients prescribed Plavix for conditions like preventing heart attacks or strokes might also have hypertension. In such cases, doctors prescribe separate blood pressure medications along with Plavix. Managing both conditions requires careful monitoring and customized treatment plans.
Consult Your Doctor
Always discuss your medications with your healthcare provider. They can accurately assess your individual needs and create a treatment strategy that addresses both your blood pressure and clotting risk effectively. Self-treating can be dangerous. Do not adjust dosages without consulting a medical professional. Proper medical advice ensures optimal health outcomes.
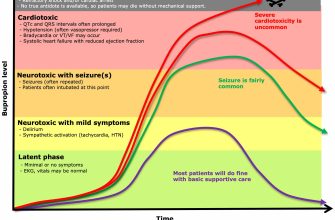
Indirect Effects on Blood Pressure: Potential Interactions with Other Medications
Clopidogrel (Plavix) doesn’t directly lower blood pressure; however, its interaction with other medications can influence blood pressure levels. Understanding these interactions is key to safe and effective treatment.
Interactions Affecting Blood Pressure
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Ibuprofen and naproxen can reduce the effectiveness of Plavix and potentially raise blood pressure. Consult your doctor before combining these.
- ACE Inhibitors & ARBs (Angiotensin-Converting Enzyme Inhibitors & Angiotensin Receptor Blockers): While not directly interacting with Plavix, these medications, commonly used for high blood pressure, work synergistically to reduce cardiovascular risk. Your doctor will monitor your blood pressure closely.
- Diuretics: These medications increase urine production, lowering blood volume and blood pressure. Concurrent use with Plavix requires careful blood pressure monitoring, as diuretics can cause dehydration.
- Proton Pump Inhibitors (PPIs): Some studies suggest PPIs like omeprazole may reduce Plavix’s effectiveness. Your doctor might suggest alternatives if you need both medications.
Managing Potential Interactions
Open communication with your doctor is paramount. Provide a complete list of all medications, supplements, and herbal remedies you are taking. Regular blood pressure monitoring helps your doctor adjust your medication regimen to minimize potential interactions and optimize your health.
Specific Recommendations
- Always inform your doctor or pharmacist about all medications you’re taking before starting Plavix.
- Regularly monitor your blood pressure as directed by your healthcare provider.
- Report any unusual symptoms, like dizziness or lightheadedness, immediately to your doctor.
- Never stop taking Plavix or any other medication without consulting your doctor.
Further Information
For detailed information about drug interactions, consult your doctor or refer to reputable medical databases like those from the FDA or your national health authority.
Cases Where Blood Pressure Might Be Affected: Specific Patient Conditions
Clopidogrel (Plavix) primarily affects blood clotting, not directly blood pressure. However, certain patient conditions can influence how Plavix interacts with blood pressure, either directly or indirectly. Let’s examine these scenarios.
- Patients with existing hypertension: Plavix alone is unlikely to significantly lower blood pressure in patients already taking hypertension medication. However, the combination of Plavix and blood pressure-lowering drugs might necessitate dosage adjustments, requiring close monitoring by your doctor. Regular blood pressure checks are crucial.
- Patients with coronary artery disease (CAD): Plavix is frequently prescribed for CAD patients. While it doesn’t directly reduce blood pressure, its impact on blood clotting reduces the risk of cardiovascular events, potentially indirectly influencing blood pressure parameters in some individuals over the long term. Consult your physician to understand the implications for your specific situation.
- Patients with peripheral artery disease (PAD): Similar to CAD, Plavix’s effect on blood clotting in PAD patients may lead to less plaque buildup, improving blood flow and potentially impacting blood pressure readings over time. Your doctor will determine the appropriate monitoring strategy.
- Patients with prior stroke or transient ischemic attack (TIA): In these cases, Plavix’s role is primarily to prevent further clotting events. The impact on blood pressure, if any, is usually indirect and secondary to improved blood flow and reduced risk of another stroke. Your doctor will monitor your blood pressure as part of your overall health assessment.
- Patients with impaired kidney function: Plavix metabolism can be affected by kidney function. This may require dosage adjustments, influencing how the medication interacts with other medications, potentially affecting blood pressure management. Close monitoring of kidney function and blood pressure is necessary.
- Patients taking other medications: Interactions with other drugs, including blood pressure medications, are possible. Always inform your physician of all medications you take, including over-the-counter drugs and supplements, to avoid adverse effects or interactions.
Remember: This information is for educational purposes only and does not substitute professional medical advice. Always discuss any concerns regarding Plavix and your blood pressure with your doctor or other qualified healthcare provider. They can assess your specific medical history and provide personalized guidance.
Monitoring Blood Pressure While on Plavix: Importance of Regular Checkups
Schedule regular blood pressure checks with your doctor. Aim for at least yearly checkups, or more frequently if advised.
Home monitoring can supplement these visits. Use a validated home blood pressure monitor and record readings consistently, ideally at the same time each day. Share these readings with your doctor at each appointment.
Consistent monitoring helps detect any unexpected changes. Early detection allows for prompt adjustments to your medication or lifestyle, helping maintain optimal blood pressure levels.
Report any significant blood pressure fluctuations, such as persistently high or low readings, to your doctor immediately. Don’t wait for your scheduled appointment.
Your doctor might suggest more frequent checkups based on your individual health profile and response to Plavix. Follow their recommendations carefully.
Maintaining a healthy lifestyle–including regular exercise, a balanced diet, and stress management–can also positively impact blood pressure. Discuss lifestyle modifications with your healthcare provider.
Remember, consistent blood pressure monitoring, combined with open communication with your doctor, is key to managing your health while taking Plavix.
Alternative Medications for Blood Pressure Management: When Plavix Isn’t Enough
If Plavix isn’t adequately controlling your blood pressure, your doctor might recommend adding other medications. Common choices include ACE inhibitors (like lisinopril or ramipril), angiotensin receptor blockers (ARBs, such as valsartan or losartan), beta-blockers (like metoprolol or atenolol), or calcium channel blockers (such as amlodipine or diltiazem).
ACE inhibitors and ARBs work by relaxing blood vessels. Beta-blockers slow your heart rate, reducing the force of contractions. Calcium channel blockers prevent calcium from entering heart muscle cells and blood vessel walls, leading to relaxation. Your doctor will consider your individual health status and other medications to select the best combination.
Lifestyle changes remain crucial. Regular exercise, a balanced diet low in sodium, and stress management techniques can significantly impact blood pressure. Aim for at least 150 minutes of moderate-intensity aerobic activity per week. Reducing sodium intake to less than 2,300 milligrams daily is recommended. Consider techniques like yoga or meditation for stress relief.
Close monitoring is key. Regular blood pressure checks help your doctor assess the efficacy of your treatment plan and make necessary adjustments. Report any side effects immediately. Open communication with your healthcare provider ensures optimal blood pressure management.
Remember, this information is for general knowledge and shouldn’t replace advice from a medical professional. Always consult your doctor before starting or changing medications or treatment plans.
Consult Your Doctor: Personalized Advice for Your Health
Schedule a consultation to discuss your blood pressure and the potential impact of Plavix. Your doctor will assess your overall health, including any existing conditions like heart disease or kidney problems.
Understanding Your Individual Needs
They’ll review your medical history and current medications. This includes not just Plavix, but also other drugs you’re taking, as interactions are possible. Blood tests may be necessary to monitor your platelet count and kidney function. Your doctor will tailor advice based on these findings.
Making Informed Decisions
Discuss your concerns and questions openly. Ask about the risks and benefits of Plavix specifically for you. Explore alternative treatment options if necessary. Remember, proactive communication is key to successful management of your health.
Monitoring and Follow-Up
Regular check-ups allow your doctor to monitor your blood pressure and adjust your treatment plan as needed. This ensures your health remains stable and you receive the best possible care. Don’t hesitate to contact your doctor between appointments if you have any questions or concerns.
Lifestyle Modifications
Your doctor can guide you on lifestyle changes to support healthy blood pressure, such as dietary adjustments, regular exercise, and stress management techniques. These modifications, combined with medication, can significantly improve your outcomes.