Regular monitoring of your white blood cell (WBC) count is critical when taking clozapine. This isn’t just a formality; it’s a life-saving precaution. Failure to adhere to this protocol significantly increases your risk of agranulocytosis, a potentially fatal condition characterized by a dangerously low WBC count.
Baseline WBC counts should be obtained before initiating clozapine therapy. Thereafter, weekly monitoring is mandated for the first six months. Following this, the frequency typically reduces to bi-weekly checks for the next six months, then monthly thereafter. Your physician will determine the precise schedule based on your individual health profile and response to treatment.
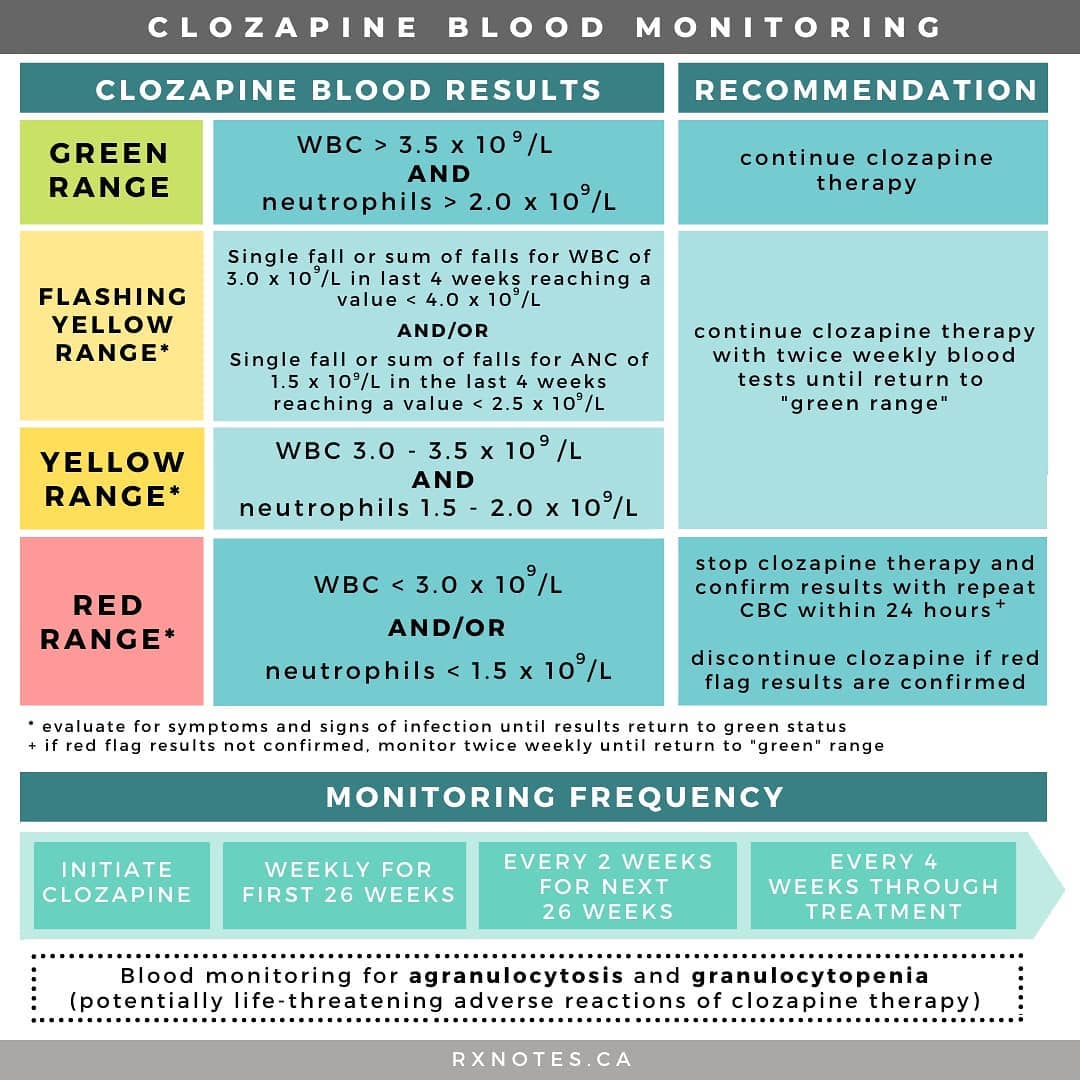
Immediate medical attention is required if your WBC count falls below 3.0 x 109/L. This is the threshold for serious concern, and prompt action can be the difference between a full recovery and severe complications. Discuss any symptoms like fever, sore throat, or unusual fatigue with your doctor without delay–these can indicate a drop in WBC count.
Remember: Consistent communication with your healthcare provider is paramount. They will provide guidance on interpreting your results and adjusting your treatment plan as needed. Active participation in your care ensures your safety and the effectiveness of your clozapine treatment.
- Clozapine and WBC Monitoring: A Practical Guide
- Understanding the Risk of Agranulocytosis
- Frequency and Timing
- Recognizing the Signs
- Monitoring Strategies
- Managing the Risk
- Alternative Treatments
- Conclusion
- Implementing Effective WBC Monitoring Protocols
- Managing Clozapine Therapy in the Context of WBC Abnormalities
Clozapine and WBC Monitoring: A Practical Guide
Begin WBC monitoring before initiating clozapine treatment. Baseline counts should be obtained within one week prior to starting therapy.
Monitor WBC counts weekly for the first six months. This frequent monitoring is critical during the initial phase of treatment due to the higher risk of agranulocytosis.
After six months of stable WBC counts, monitoring frequency can be reduced to bi-weekly for the next six months. Consistent, normal counts allow for less frequent checks.
Once a year of stable, normal WBC counts are documented, monthly monitoring is sufficient. This schedule provides ongoing surveillance while minimizing inconvenience.
Absolute neutrophil count (ANC) is the most relevant measurement. Focus on this specific value rather than solely relying on the total WBC count.
Discontinue clozapine immediately if the ANC falls below 1500/µL. Prompt action is vital to prevent severe complications.
Closely collaborate with a hematologist. Their expertise is crucial for interpreting results and managing potential complications.
Document all WBC and ANC values meticulously. Maintain accurate records for both patient safety and regulatory compliance.
Educate patients about the importance of regular blood tests and potential side effects. Open communication improves adherence and safety.
Consider the patient’s overall health and other medications when interpreting results. Context is key to accurate assessment.
Regularly review the patient’s clinical response to clozapine alongside the blood count results. This holistic approach allows for informed decision-making.
Understanding the Risk of Agranulocytosis
Agranulocytosis, a severe drop in white blood cells, is a serious side effect of clozapine. This reduction significantly weakens your immune system, leaving you vulnerable to infections.
Frequency and Timing
Agranulocytosis occurs in approximately 1% of patients taking clozapine. It typically develops within the first 18 weeks of treatment, although it can occur later. Regular monitoring is vital during this period, and even after that, continued vigilance is advised.
Recognizing the Signs
Pay close attention to potential symptoms. These include:
- Sore throat
- Fever
- Chills
- Weakness
- Mouth sores
- Easy bruising or bleeding
If you experience any of these, seek immediate medical attention. Early detection and treatment are critical.
Monitoring Strategies
Your doctor will schedule regular blood tests to monitor your white blood cell count (WBC). The frequency of these tests will depend on various factors, such as your individual risk profile and response to treatment. Adherence to this schedule is paramount for your safety.
Managing the Risk
- Consistent Monitoring: Regular WBC counts are the cornerstone of safe clozapine use.
- Prompt Reporting: Report any symptoms suggestive of infection immediately to your healthcare provider.
- Open Communication: Maintain open communication with your doctor about any concerns or changes in your health.
Alternative Treatments
If agranulocytosis develops, clozapine will be stopped immediately. Your healthcare provider will discuss alternative treatment options.
Conclusion
While agranulocytosis is a serious risk, proactive monitoring and prompt action greatly reduce the likelihood of severe complications. Your active participation in your care is essential.
Implementing Effective WBC Monitoring Protocols
Establish a baseline WBC count before initiating clozapine therapy. Frequency of monitoring should align with clinical guidelines and patient risk factors. For instance, weekly monitoring is often recommended during the initial six months, transitioning to bi-weekly or monthly checks thereafter, based on stability.
Use a standardized blood collection and testing protocol to minimize variability. Clearly define acceptable ranges for WBC counts and establish triggers for dose adjustments or temporary clozapine discontinuation. These thresholds should be documented and readily accessible to all healthcare providers.
Employ a robust electronic health record (EHR) system to manage and track WBC data, ensuring timely alerts and notifications to the healthcare team when critical values are detected. This system should facilitate immediate communication with the patient and their support network.
Educate patients and their caregivers about the importance of regular blood tests and potential side effects, empowering them to actively participate in their care. Provide clear instructions about reporting symptoms such as fever, sore throat, or unusual bruising.
Regularly review and update your WBC monitoring protocols based on the latest clinical evidence and best practice guidelines. This ensures adherence to current standards and minimizes risk.
Implement a system for documenting and analyzing WBC trends to facilitate timely identification of potential agranulocytosis. This may involve the use of graphical representations of WBC counts over time. Promptly address any concerns related to declining WBC counts.
Collaborate closely with hematologists or other relevant specialists for complex cases or when managing patients with pre-existing hematological conditions. A multidisciplinary approach ensures optimal patient care.
Managing Clozapine Therapy in the Context of WBC Abnormalities
Begin by immediately suspending clozapine upon detection of a white blood cell (WBC) count below 3.0 x 109/L or an absolute neutrophil count (ANC) below 1.5 x 109/L. Closely monitor the patient’s WBC and ANC counts daily until they recover. This includes daily blood tests.
Regular monitoring is key. Aim for weekly WBC and ANC checks during the first six months of treatment, then bi-weekly for the next six months, and then monthly thereafter, as long as counts remain stable. Adjust monitoring frequency based on individual patient response and risk profile.
A structured approach to managing these abnormalities is crucial. Consider these guidelines:
| WBC Count (x 109/L) | ANC Count (x 109/L) | Action |
|---|---|---|
| ≥3.0 | ≥1.5 | Continue clozapine, maintain monitoring schedule |
| 2.0 – 2.9 | 1.0 – 1.4 | Reduce clozapine dose, increase monitoring frequency to daily counts. Consult hematologist. |
| <2.0 | <1.0 | Discontinue clozapine, initiate supportive care, consult hematologist immediately. |
Close collaboration with a hematologist is necessary throughout the process. They provide expert guidance on managing hematological complications and help determine when and how to safely resume clozapine therapy following recovery. Document all blood count results and any actions taken meticulously in the patient’s medical record. Explain risks and benefits to the patient clearly, fostering informed decision-making.
Remember that prompt action is critical for minimizing the risk of serious complications. Carefully weigh the benefits of clozapine against the potential risks of hematological side effects. Individual patient factors, including other health conditions and medication interactions, should be considered. A patient’s clinical response to clozapine must be regularly assessed to help make informed decisions about the treatment.