Experiencing knee pain after taking Cipro? You’re not alone. Many individuals report tendon damage as a side effect of this antibiotic. This article clarifies the connection and provides actionable advice.
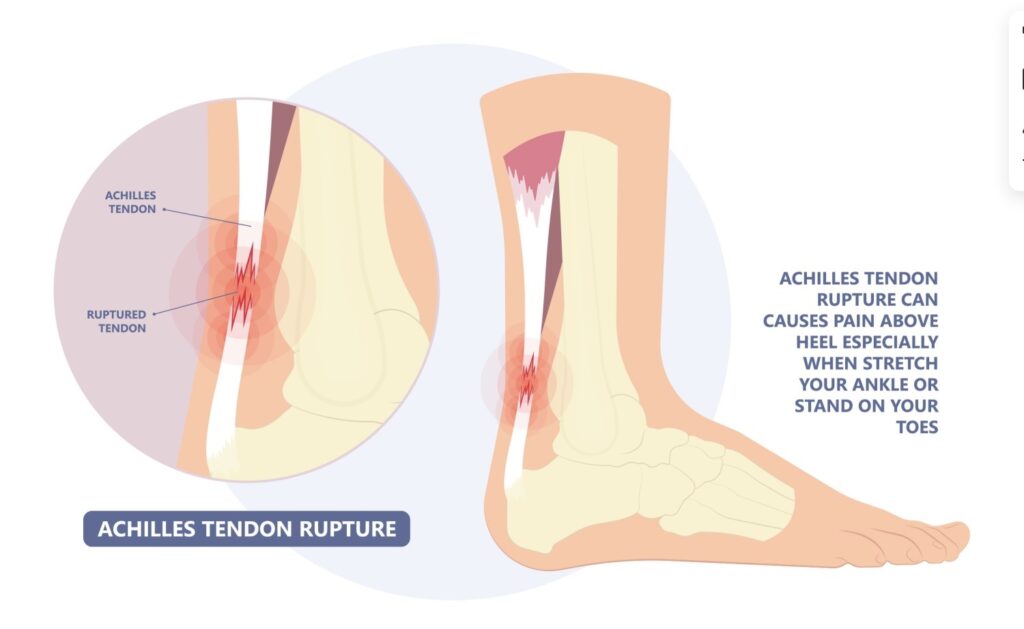
Ciprofloxacin, the active ingredient in Cipro, has been linked to tendinitis and tendon rupture, particularly affecting the Achilles tendon but also impacting knees. Reports suggest a higher risk for individuals over 60 and those already susceptible to tendon injuries. This isn’t a guaranteed outcome, but understanding the potential risk is vital.
Early detection is key. If you experience knee pain, swelling, or stiffness after starting Cipro, immediately contact your doctor. Don’t attempt self-diagnosis or delay seeking professional medical attention. Your physician can assess your condition and recommend appropriate management strategies, potentially including physical therapy or medication changes.
Remember, this information aims to inform, not replace, medical advice. Always consult with your healthcare provider for personalized guidance regarding your health concerns.
- Knee Problems from Cipro: A Detailed Overview
- Understanding Ciprofloxacin and its Mechanism
- Targeting Bacterial Enzymes
- Factors Affecting Ciprofloxacin’s Action
- Common Knee Problems Associated with Cipro Use
- Risk Factors and Predisposing Conditions
- Diagnosis and Treatment Options for Cipro-Induced Knee Pain
- Preventing Cipro-Related Knee Issues: Strategies and Precautions
Knee Problems from Cipro: A Detailed Overview
Ciprofloxacin (Cipro) can cause tendon damage, including in the knees. This risk is increased with age, high doses, and pre-existing conditions like kidney disease. Symptoms might include pain, swelling, and stiffness. See a doctor immediately if you experience these.
While not everyone taking Cipro experiences knee problems, studies indicate a statistically significant increase in tendon rupture risk. This risk is generally considered low but warrants attention. Certain factors increase this risk, including steroid use concurrent with Cipro.
Diagnosis usually involves a physical examination and may include imaging tests like MRI or ultrasound. Treatment focuses on rest, pain management (e.g., NSAIDs), and physical therapy to aid recovery. Surgical repair might be necessary in cases of tendon rupture.
Prevention is key. Discuss your medical history thoroughly with your doctor before starting Cipro. If you’re over 60, have a history of tendon problems, or are taking steroids, the risks are higher. Carefully weigh the benefits against the potential risks of Cipro.
Alternatives to Cipro exist. Discuss these options with your healthcare provider. They can consider your specific condition and prescribe an antibiotic with a lower risk of tendon damage, if appropriate.
Complete recovery time varies greatly, depending on the severity of the damage and individual factors. Consistent adherence to your doctor’s treatment plan, including physical therapy, is vital for optimal healing.
Remember, this information is for educational purposes only and does not constitute medical advice. Always consult with a healthcare professional for diagnosis and treatment of any medical condition.
Understanding Ciprofloxacin and its Mechanism
Ciprofloxacin targets bacterial DNA gyrase and topoisomerase IV. These enzymes are crucial for bacterial DNA replication, repair, and segregation. Ciprofloxacin inhibits these enzymes, preventing bacteria from properly replicating their DNA, ultimately leading to cell death.
Targeting Bacterial Enzymes
Specifically, ciprofloxacin binds to these enzymes, altering their structure and preventing them from functioning correctly. This mechanism differs significantly from how many other antibiotics work, making it effective against a wide range of bacteria, including gram-negative and some gram-positive organisms. The drug’s effectiveness depends on the concentration achieved at the infection site and the susceptibility of the bacteria. Resistance can develop through mutations in the target enzymes.
Factors Affecting Ciprofloxacin’s Action
Several factors influence how well ciprofloxacin works. These include the specific bacterial species involved, the dose of the medication, the route of administration (oral versus intravenous), and the patient’s individual metabolism. Proper dosage and duration of treatment are therefore critical for successful outcomes. A doctor’s guidance is necessary for prescribing and managing ciprofloxacin use to minimize potential adverse effects.
Common Knee Problems Associated with Cipro Use
Ciprofloxacin, a common antibiotic, can sometimes cause tendon damage, frequently affecting the knees. This manifests in several ways.
- Tendinitis: This is inflammation of the tendon, causing pain, swelling, and stiffness in your knee. You might experience tenderness to the touch along the tendon.
- Tendon rupture: In more severe cases, the tendon can completely tear. This results in sudden, intense knee pain, often accompanied by noticeable swelling and an inability to bear weight on the leg. Seek immediate medical attention if this occurs.
- Pain and stiffness: Even without a full rupture or diagnosed tendinitis, many individuals report persistent knee pain and stiffness following Cipro use. This pain can range from mild discomfort to significant limitation in mobility.
The risk of these problems is higher in certain groups: older adults, individuals already suffering from tendon issues, and those taking corticosteroids concurrently.
If you experience knee pain after taking Cipro, promptly consult your doctor. They can provide a proper diagnosis and recommend appropriate treatment, which might involve rest, ice, physical therapy, or other interventions. Early diagnosis can improve recovery outcomes.
- Rest and Ice: Reduce activity and apply ice packs to the affected area to minimize swelling and pain.
- Over-the-counter pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen may help manage pain and inflammation.
- Physical Therapy: A physical therapist can develop a customized exercise program to strengthen the knee and improve its range of motion.
Remember, this information is for general knowledge and does not replace professional medical advice. Always discuss any health concerns with a doctor.
Risk Factors and Predisposing Conditions
Individuals with pre-existing knee conditions like osteoarthritis or previous knee injuries face a heightened risk of Cipro-related tendon damage. Age also plays a significant role; older adults are more susceptible.
Concurrent use of corticosteroids, such as prednisone, dramatically increases the likelihood of tendon rupture. This is due to the synergistic effect of both drugs on tendon strength.
High-intensity physical activity increases stress on tendons, making individuals more vulnerable to Cipro’s tendon-damaging effects. Consider modifying exercise routines while taking the medication.
Kidney or liver impairment can affect how the body processes Cipro, potentially raising the risk of adverse effects. Always inform your doctor about any existing health issues.
Genetic predisposition might contribute to individual susceptibility. Research suggests variations in genes involved in collagen metabolism could influence tendon health and Cipro response.
While rare, certain medical conditions, such as lupus or rheumatoid arthritis, might increase sensitivity to Cipro’s side effects on tendons. Discuss your medical history thoroughly with your doctor before beginning treatment.
Diagnosis and Treatment Options for Cipro-Induced Knee Pain
Confirming Cipro-induced tendinitis requires a thorough medical history review, focusing on Ciprofloxacin use and the onset of knee pain. Your doctor will perform a physical exam, checking for tenderness, swelling, and limited range of motion. Imaging studies, such as X-rays, may rule out other causes. Sometimes, blood tests may be used to identify inflammation markers.
Treatment prioritizes pain relief and healing. Rest is crucial; avoid activities that aggravate your knee. Over-the-counter pain relievers like ibuprofen or naproxen can help manage pain and inflammation. Your doctor might prescribe stronger analgesics or corticosteroids for severe cases.
Physical therapy plays a vital role. A physical therapist designs a program of exercises to improve strength, flexibility, and range of motion, gradually increasing the intensity. They’ll also teach you proper techniques to avoid re-injury.
In some instances, your doctor may recommend other interventions. These could include:
| Intervention | Description |
|---|---|
| Bracing or Splinting | Provides support and stability to the knee joint. |
| Corticosteroid Injections | Reduces inflammation directly in the affected area. |
| Surgery | Rarely needed, reserved for cases with severe tendon rupture or persistent symptoms. |
Time is a factor in healing. Complete recovery can take weeks or months, depending on the severity of the tendinitis. Following your doctor’s and physical therapist’s recommendations diligently is vital for optimal outcomes. Remember to report any worsening symptoms immediately.
Preventing Cipro-Related Knee Issues: Strategies and Precautions
Maintain adequate hydration. Drink plenty of water throughout your Ciprofloxacin treatment. Proper hydration helps your body process the medication and may reduce the risk of tendon damage.
Prioritize regular, low-impact exercise. Gentle activities like walking or swimming strengthen muscles supporting your knees, promoting joint health during and after treatment.
Listen to your body. Rest when you experience knee pain or stiffness. Ignoring discomfort can worsen the problem. Don’t push yourself beyond your limits.
Consult your doctor about alternative antibiotics. If you have a history of tendonitis or other knee problems, discuss alternative treatment options with your physician before starting Ciprofloxacin.
Take Ciprofloxacin exactly as prescribed. Strictly follow your doctor’s instructions regarding dosage and duration of treatment. Avoid exceeding the recommended dose.
Report any knee pain or swelling immediately. Prompt reporting allows for early intervention and may help prevent further complications. Contact your doctor or seek medical attention without delay.
Consider glucosamine and chondroitin supplements. While research is ongoing, some studies suggest these supplements may support joint health. Discuss their use with your doctor before taking them, especially if you are taking other medications.