Medroxyprogesterone acetate (MPA) isn’t typically prescribed for COPD. Current treatment guidelines focus on bronchodilators, inhaled corticosteroids, and sometimes antibiotics for exacerbations. However, research suggests a potential role for MPA in specific COPD subsets. This exploration will clarify its limited applicability.
Some studies hint at MPA’s impact on inflammatory processes relevant to COPD. This is because it’s a progestin and possesses anti-inflammatory properties. However, its use remains controversial. Direct clinical evidence supporting its routine use in COPD management is lacking. Further research is needed before any definitive recommendation can be made.
Important Note: If you’re considering MPA for COPD, discuss it thoroughly with your doctor. They can assess your individual needs, risk factors, and response to other treatments to determine if it’s appropriate for you. Never adjust your medication without consulting your physician. Self-medicating can be dangerous and may compromise your health.
Always prioritize established COPD therapies. MPA’s potential benefits need further investigation and shouldn’t replace proven treatments. Focus on adhering to your doctor’s treatment plan, which includes pulmonary rehabilitation, smoking cessation if applicable, and proper medication management.
- Medroxyprogesterone for COPD: A Detailed Overview
- MPA’s Potential Role in COPD
- Considerations and Cautions
- Medroxyprogesterone’s Mechanism of Action in COPD
- Impact on Inflammatory Pathways
- Potential Benefits and Limitations
- Current Clinical Evidence Supporting or Refuting Medroxyprogesterone Use in COPD
- Potential Benefits and Risks Associated with Medroxyprogesterone Treatment for COPD
- Potential Benefits
- Potential Risks
- Alternative and Complementary Therapies for COPD Management
- Practical Considerations for Patients Considering Medroxyprogesterone for COPD
- Medication Interactions
- Potential Side Effects
- Monitoring and Follow-Up
- Lifestyle Changes
- Alternative Treatments
- Cost and Insurance
Medroxyprogesterone for COPD: A Detailed Overview
Medroxyprogesterone acetate (MPA) isn’t a standard treatment for COPD. Current guidelines prioritize bronchodilators, inhaled corticosteroids, and pulmonary rehabilitation. However, research suggests a potential role for MPA in specific COPD subpopulations, warranting further discussion.
MPA’s Potential Role in COPD
Some studies indicate MPA might help manage certain COPD symptoms, particularly those linked to inflammation and dyspnea (shortness of breath). The mechanism isn’t fully understood but may involve its anti-inflammatory properties and impact on airway reactivity. It’s crucial to remember this isn’t a first-line therapy. Its use should be considered only after other treatment strategies have been exhausted.
Considerations and Cautions
The benefits of MPA in COPD are limited and require careful evaluation. Potential side effects, including weight gain, mood changes, and increased risk of thromboembolic events, must be weighed against any potential therapeutic advantages. Regular monitoring is essential. Furthermore, MPA interacts with several medications commonly used in COPD management, necessitating careful medication reconciliation.
| Potential Benefit | Potential Side Effect | Monitoring Needs |
|---|---|---|
| Reduced dyspnea in some patients | Weight gain | Regular weight checks |
| Improved inflammatory markers (in some studies) | Mood changes (depression, anxiety) | Mood assessments |
| N/A | Increased risk of blood clots | Regular blood tests |
Always discuss the use of MPA with your pulmonologist or healthcare provider. They can assess your individual circumstances, considering your COPD severity, other health conditions, and current medications, to determine if MPA is appropriate. Self-medicating is strongly discouraged.
Medroxyprogesterone’s Mechanism of Action in COPD
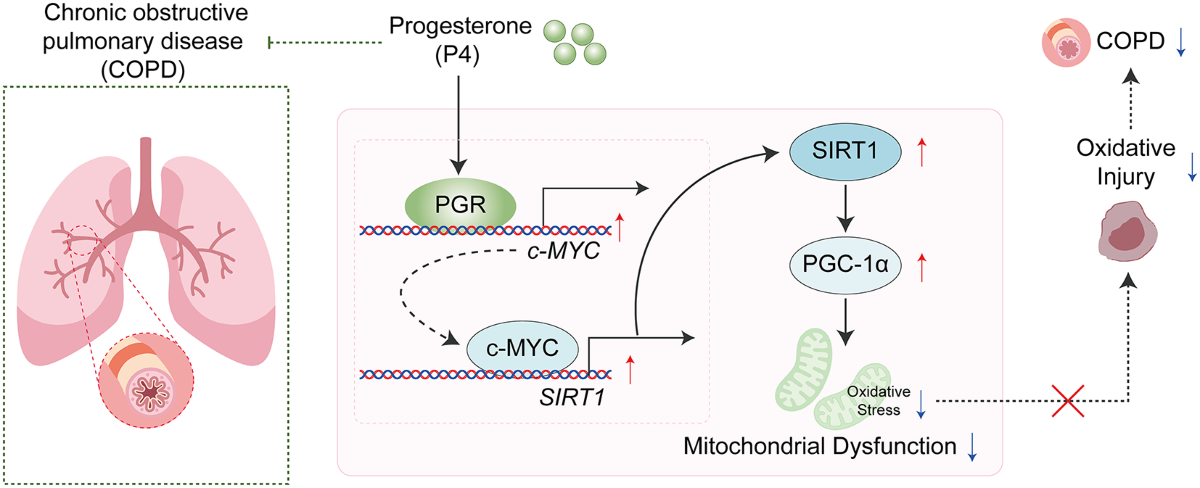
Medroxyprogesterone acetate (MPA), a synthetic progestin, doesn’t directly treat the underlying inflammation in COPD. Its potential benefit stems from its anti-inflammatory and immunomodulatory properties. Specifically, MPA might reduce the production of pro-inflammatory cytokines like TNF-α and IL-6, key players in COPD exacerbation. This action could lead to lessened airway inflammation and improved lung function.
Impact on Inflammatory Pathways
Studies suggest MPA influences several pathways contributing to COPD pathogenesis. It interacts with glucocorticoid receptors, although less potently than true glucocorticoids. This interaction might augment the anti-inflammatory effects of corticosteroids, already a cornerstone of COPD management. Further research is needed to fully understand the extent of this interaction and clarify the precise mechanisms involved in reducing inflammation.
Potential Benefits and Limitations
While preclinical and some clinical data hint at potential benefits, the evidence for MPA’s use in COPD remains limited. Current recommendations don’t include MPA as a first-line treatment. However, ongoing research might reveal a role for MPA in specific COPD subgroups, particularly those experiencing frequent exacerbations or those unresponsive to standard therapies. More robust clinical trials are necessary to definitively establish its efficacy and safety in this context.
Current Clinical Evidence Supporting or Refuting Medroxyprogesterone Use in COPD
Currently, there’s limited high-quality evidence directly supporting the use of medroxyprogesterone in treating COPD. Most research focuses on its effects in other conditions.
Studies exploring medroxyprogesterone’s impact on respiratory function in COPD patients are scarce. Existing literature primarily consists of case reports and small observational studies, hindering definitive conclusions regarding efficacy and safety.
- A 2018 case report suggested potential benefits in reducing dyspnea in a single patient, but this needs confirmation through larger, controlled trials.
- Several studies examine medroxyprogesterone’s impact on other aspects of COPD, like cachexia (muscle wasting), but results are inconclusive and require further investigation.
Concerns exist regarding potential adverse effects, including:
- Increased risk of thromboembolic events.
- Weight gain.
- Mood changes.
Therefore, prescribing medroxyprogesterone for COPD should be approached with caution. It’s not currently considered a standard treatment. More robust clinical trials are needed before any recommendation for routine use can be made.
Clinicians should prioritize evidence-based therapies for COPD management, focusing on bronchodilators, inhaled corticosteroids, and pulmonary rehabilitation. If considering medroxyprogesterone for a specific symptom (e.g., cachexia), a thorough risk-benefit assessment is crucial, potentially involving a multidisciplinary team.
- Prioritize established COPD treatments.
- Consider medroxyprogesterone only after careful evaluation and with close monitoring for side effects.
- Advocate for further research on medroxyprogesterone’s role in COPD management.
Potential Benefits and Risks Associated with Medroxyprogesterone Treatment for COPD
Medroxyprogesterone acetate (MPA) isn’t a standard COPD treatment. Research suggests potential benefits in specific COPD subsets, primarily those experiencing severe dyspnea (shortness of breath) linked to hyperinflation. This is because MPA might reduce airway inflammation and improve lung mechanics in some patients.
Potential Benefits
Studies show MPA may alleviate dyspnea in certain COPD patients through its anti-inflammatory properties. However, these effects are not consistently observed across all studies, and more research is needed to confirm these findings and understand the mechanisms involved.
Potential Risks
MPA carries potential side effects including weight gain, mood changes, thromboembolic events (blood clots), and increased risk of endometrial cancer in women. Men may experience decreased libido. These risks must be carefully weighed against any potential benefits before considering MPA therapy for COPD. Regular monitoring is crucial.
Important Note: MPA is not a first-line treatment for COPD. Its use should be restricted to carefully selected patients under close medical supervision, and only after discussion of the potential benefits and risks with a healthcare professional. Standard COPD management, including bronchodilators, inhaled corticosteroids, and pulmonary rehabilitation, should remain the foundation of treatment.
Alternative and Complementary Therapies for COPD Management
Pulmonary rehabilitation significantly improves exercise capacity and quality of life. Consider a program incorporating supervised exercise, education, and breathing techniques.
Oxygen therapy increases blood oxygen levels, easing breathlessness. Discuss oxygen prescription with your doctor to determine the appropriate flow rate and duration.
Bronchodilator medications, like inhaled beta-agonists and anticholinergics, relax airway muscles, improving airflow. Follow your doctor’s instructions carefully regarding dosage and timing.
Mindfulness and meditation techniques can reduce stress and anxiety, which often exacerbate COPD symptoms. Explore guided meditation apps or local classes.
Acupuncture may help manage pain and improve breathing. Seek a qualified and licensed practitioner with experience treating respiratory conditions.
Dietary changes focusing on nutrient-rich foods and adequate hydration support overall health and lung function. Consult a registered dietitian for personalized dietary recommendations.
Chest physiotherapy techniques, such as percussion and postural drainage, help clear mucus from the lungs. Learn these techniques from a respiratory therapist.
Tai chi and yoga improve lung function, flexibility, and overall well-being through gentle movements and controlled breathing exercises. Find a class suited to your fitness level.
Always discuss any alternative or complementary therapies with your physician before starting them, ensuring they won’t interact negatively with your prescribed medications or underlying health conditions.
Practical Considerations for Patients Considering Medroxyprogesterone for COPD
Discuss all treatment options with your doctor. Medroxyprogesterone is not a first-line COPD treatment; its use is very specific. Understand its role and limitations before proceeding.
Medication Interactions
Inform your doctor about all medications you take, including over-the-counter drugs and supplements. Medroxyprogesterone can interact with other drugs, potentially altering their effectiveness or causing adverse effects. Your doctor will help determine potential conflicts and adjust your medication regimen accordingly.
Potential Side Effects
Be aware of possible side effects like weight gain, mood changes, and menstrual irregularities. These can vary in severity. Report any concerning symptoms promptly to your healthcare provider. They can offer strategies for managing these side effects or suggest alternative treatments if necessary.
Monitoring and Follow-Up
Regular check-ups are vital. Your doctor will monitor your response to the medication and adjust the dosage if needed. Consistent monitoring helps ensure the medication’s efficacy and minimizes potential risks. Open communication with your physician is key to successful treatment.
Lifestyle Changes
Medroxyprogesterone alone won’t cure COPD. Maintain a healthy lifestyle through proper nutrition, regular exercise (as tolerated), and smoking cessation (if applicable). These lifestyle modifications significantly improve COPD management and overall health.
Alternative Treatments
Explore alternative treatments if Medroxyprogesterone proves ineffective or produces unacceptable side effects. Your physician can discuss other options, such as bronchodilators, corticosteroids, or pulmonary rehabilitation, to better manage your COPD.
Cost and Insurance
Discuss the medication’s cost and insurance coverage beforehand. Explore options to mitigate financial burdens if necessary. Your doctor or a healthcare professional can provide assistance with accessing affordable medication.