Need an alternative to amoxicillin? Consider azithromycin, a macrolide antibiotic often prescribed for similar bacterial infections. Azithromycin offers a convenient dosage regimen – typically a shorter course of treatment. Remember to always consult your doctor before switching medications.
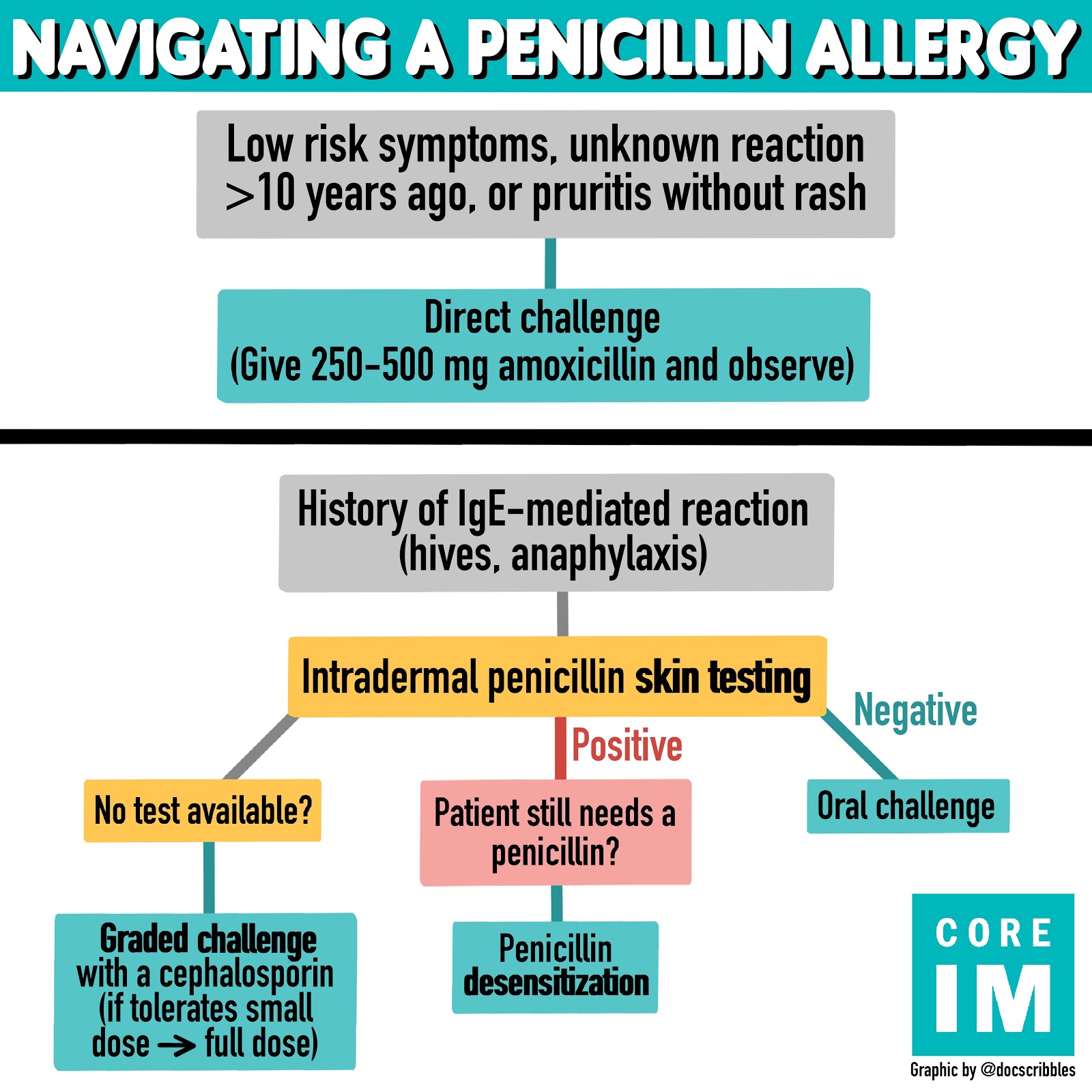
If you have a penicillin allergy, cephalosporins such as cefuroxime might be suitable. However, cross-reactivity is possible; discuss your allergy history thoroughly with your physician to determine the safest option. They can perform allergy testing if necessary to ensure the choice is appropriate for you.
For certain infections, alternative antibiotics like doxycycline (a tetracycline) or clindamycin (a lincosamide) could be effective. These are often used for respiratory or skin infections. The choice depends on the specific bacteria causing your illness and your medical history. Your doctor will make the best recommendation based on your individual needs.
Always seek professional medical advice before starting any new medication, including alternative antibiotics. Self-treating can be harmful and delay proper treatment of your condition. Your doctor will conduct a thorough assessment and choose the most appropriate and safe antibiotic for you.
- Alternative for Amoxicillin
- Alternatives for Common Infections
- Factors Influencing the Choice
- Understanding Amoxicillin’s Limitations
- Resistance: A Growing Concern
- Side Effects: A Balance of Risks and Benefits
- Specific Infections: Amoxicillin’s Ineffectiveness
- Alternatives: Exploring Other Options
- Penicillins: Similar Alternatives to Amoxicillin
- Cephalosporins: A Broader-Spectrum Option
- Macrolides: Effective Against Similar Bacteria
- Choosing the Right Alternative: Consulting Your Doctor
- When to Seek Alternative Treatment for Amoxicillin Resistance
Alternative for Amoxicillin
Your doctor should guide your treatment, but knowing options is helpful. Amoxicillin’s alternatives depend on the infection. For bacterial infections, consider these possibilities:
Alternatives for Common Infections
- Respiratory infections (e.g., bronchitis, pneumonia): Alternatives include azithromycin, clarithromycin, or doxycycline. Dosage and duration vary depending on the severity and the specific bacteria.
- Ear infections (otitis media): Cefdinir, ceftriaxone, or azithromycin can be effective. Always consult a doctor for ear infections, as delayed treatment can lead to complications.
- Skin infections (e.g., cellulitis): Cephalexin, clindamycin, or erythromycin might be prescribed. Appropriate antibiotic selection depends on the causative bacteria and the infection’s location.
- Urinary tract infections (UTIs): Nitrofurantoin, sulfamethoxazole-trimethoprim, or ciprofloxacin are common options. Proper hydration and frequent urination are vital alongside antibiotics.
Remember, these are just examples. Antibiotic choice depends on several factors, including the type of bacteria causing the infection, your medical history, and potential allergies.
Factors Influencing the Choice
- Bacterial identification: A culture and sensitivity test helps determine the best antibiotic.
- Allergies: A history of penicillin allergy often requires alternative choices.
- Severity of infection: Severe infections may require intravenous antibiotics.
- Patient-specific factors: Age, pregnancy, and other health conditions influence the decision.
Never self-medicate. Always consult a healthcare professional for diagnosis and treatment of any infection. They will consider your individual needs and prescribe the most suitable antibiotic or alternative therapy.
Understanding Amoxicillin’s Limitations
Amoxicillin, while a widely used antibiotic, isn’t a perfect solution for every bacterial infection. Its effectiveness varies depending on the specific bacteria involved. For example, it struggles against many strains of Pseudomonas aeruginosa, a bacterium commonly responsible for hospital-acquired infections.
Resistance: A Growing Concern
Antibiotic resistance is a major hurdle. Prolonged or inappropriate use of amoxicillin contributes to the development of resistant bacteria. This means that future infections might prove more difficult to treat. The rise of penicillinase-producing bacteria significantly reduces amoxicillin’s efficacy. Consider this when choosing an antibiotic.
Side Effects: A Balance of Risks and Benefits
Amoxicillin, like all medications, carries potential side effects. Common reactions include diarrhea, nausea, and skin rashes. Serious, though rare, allergic reactions can occur. Individuals with a history of penicillin allergies should avoid amoxicillin completely. Always weigh the benefits against these potential risks.
Specific Infections: Amoxicillin’s Ineffectiveness
Amoxicillin is ineffective against viral infections, such as the common cold or influenza. Using it in such cases is unnecessary and contributes to antibiotic resistance. It also may not be the best choice for treating certain bacterial infections like those caused by Mycoplasma pneumoniae or atypical pneumonia.
Alternatives: Exploring Other Options
Consult a healthcare professional to determine the most appropriate antibiotic for your specific infection. They will consider factors such as your medical history, the type of bacteria involved, and the severity of the infection before recommending an alternative. This ensures you receive the most effective treatment while minimizing the risk of complications.
Penicillins: Similar Alternatives to Amoxicillin
If amoxicillin isn’t suitable, your doctor might prescribe another penicillin. These share a similar mechanism of action but differ in how they’re absorbed and their effectiveness against specific bacteria.
Ampicillin is a broader-spectrum penicillin than amoxicillin, meaning it’s effective against a wider range of bacteria. However, it’s often associated with more side effects.
Amoxicillin/clavulanate (Augmentin) combines amoxicillin with clavulanic acid, which helps overcome bacterial resistance. This is a good option if amoxicillin alone is ineffective.
Dicloxacillin is a penicillin primarily used for staphylococcal infections, offering a targeted approach when those bacteria are the culprit.
Piperacillin/tazobactam (Zosyn) is a potent penicillin used for severe infections, typically those requiring intravenous administration in hospital settings. It’s not a typical first-line alternative to oral amoxicillin.
The choice of alternative depends entirely on the specific infection and your individual medical history. Always consult your doctor for appropriate treatment.
Cephalosporins: A Broader-Spectrum Option
Cephalosporins offer a viable alternative to amoxicillin, particularly when treating infections caused by bacteria resistant to penicillin. They work by interfering with bacterial cell wall synthesis, leading to bacterial death.
Several cephalosporin generations exist, each with varying effectiveness against different bacteria. First-generation cephalosporins, like cefazolin, are effective against gram-positive bacteria. Second-generation cephalosporins, including cefuroxime, broaden the spectrum to include some gram-negative bacteria. Third-generation cephalosporins, such as ceftriaxone, target a wider range of gram-negative organisms. Fourth-generation cephalosporins, like cefepime, boast even broader coverage, including some bacteria resistant to earlier generations.
Your doctor will determine the appropriate cephalosporin based on your infection’s severity and the bacteria involved. Cefazolin is often used for surgical prophylaxis, while ceftriaxone frequently treats severe infections like pneumonia or meningitis. Remember to always follow your doctor’s prescribed dosage and duration to ensure effective treatment and minimize the risk of resistance development.
Potential side effects include diarrhea, nausea, and rash. Inform your doctor immediately if you experience any serious adverse reactions. Allergic reactions, while possible, are less common than with penicillin antibiotics. However, a history of penicillin allergy should be disclosed to your physician before starting cephalosporin therapy.
While cephalosporins provide a broader spectrum of activity, they may not be suitable for all individuals or infections. Always consult a healthcare professional for accurate diagnosis and treatment recommendations.
Macrolides: Effective Against Similar Bacteria
Macrolides, such as erythromycin, azithromycin, and clarithromycin, often target similar bacteria as amoxicillin. They’re particularly useful against respiratory infections caused by Streptococcus pneumoniae, Haemophilus influenzae, and Mycoplasma pneumoniae.
However, resistance to macrolides is increasing, so it’s crucial to discuss specific bacterial sensitivities with your doctor before treatment.
| Macrolide | Common Uses | Potential Side Effects |
|---|---|---|
| Erythromycin | Respiratory infections, skin infections | Gastrointestinal upset, nausea |
| Azithromycin | Respiratory infections, sexually transmitted infections (STIs) | Diarrhea, abdominal pain |
| Clarithromycin | Respiratory infections, skin infections, stomach ulcers (caused by H. pylori) | Taste disturbances, nausea |
Your physician will consider factors like your medical history, the specific infection, and potential drug interactions when determining if a macrolide is appropriate. Always follow your doctor’s instructions regarding dosage and duration of treatment. Never self-medicate.
Note that while macrolides share some overlapping efficacy with amoxicillin, they are not interchangeable. Different antibiotics target bacteria in distinct ways, and using the incorrect antibiotic can hinder treatment.
Choosing the Right Alternative: Consulting Your Doctor
Always discuss alternative options with your doctor before making any changes to your medication. They possess the necessary expertise to assess your specific medical history, current condition, and potential drug interactions.
Your doctor will consider factors such as your allergies, other medications you’re taking, and the severity of your infection. This comprehensive assessment ensures the safest and most effective treatment plan for you.
Be prepared to provide a detailed account of your symptoms and any previous antibiotic treatments. This information helps your doctor determine the best alternative, possibly including different antibiotics, antiviral medications, or even alternative therapies depending on the infection.
Expect your doctor to explain the benefits and risks associated with each potential alternative. They will clarify how the alternative works, its potential side effects, and the expected duration of treatment.
Active participation in this discussion is key. Don’t hesitate to ask questions about potential side effects, treatment duration, and the likelihood of success. Clear communication ensures you receive the best possible care and understand your treatment plan thoroughly. Following your doctor’s recommendations is crucial for successful recovery.
When to Seek Alternative Treatment for Amoxicillin Resistance
If your symptoms persist or worsen after a full course of amoxicillin, seek alternative treatment. This includes situations where you experience:
- No improvement in symptoms after 72 hours of treatment
- Recurring or new symptoms after initial improvement
- High fever (over 101°F or 38.3°C) accompanied by severe symptoms
- Signs of a serious infection, like difficulty breathing or severe abdominal pain
Specific instances demanding immediate alternative treatment include:
- Suspected bacterial pneumonia with no improvement after 48 hours on amoxicillin
- Severe urinary tract infection (UTI) not responding to amoxicillin within 24-48 hours
- Cellulitis spreading rapidly despite amoxicillin therapy
Consider these factors when discussing alternative treatment options with your doctor:
- Your medical history, including allergies and previous antibiotic use.
- The suspected bacteria causing your infection (if known).
- Your overall health and immune system status.
- Potential side effects of alternative antibiotics.
Your doctor will assess your situation and recommend a suitable alternative, possibly including other antibiotics like azithromycin, clarithromycin, or ceftriaxone, depending on the specifics of your case. Delaying treatment for resistant infections can lead to complications, so prompt action is key. Don’t hesitate to contact your healthcare provider if you have concerns.