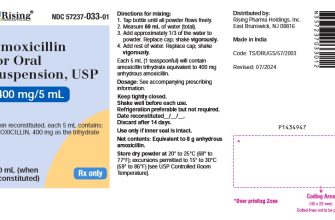
No, amoxicillin is not a treatment for bacterial vaginosis (BV). This common misconception needs clarifying. BV is caused by an imbalance of vaginal bacteria, and amoxicillin, a broad-spectrum antibiotic, targets different bacterial types. Using it for BV can disrupt your vaginal flora further, potentially worsening the condition. Instead of amoxicillin, consult your doctor.
Your doctor will likely recommend metronidazole or clindamycin, which are specifically designed to treat BV. These antibiotics effectively target the bacteria responsible for this infection. They come in various forms–creams, tablets, or oral gels–allowing your physician to choose the best approach based on your individual needs and the severity of your infection. A proper diagnosis is key before starting treatment, so schedule an appointment to discuss your symptoms.
Accurate diagnosis often involves a pelvic exam and testing of vaginal discharge to identify the presence and type of bacteria. Self-treating BV can be risky; delaying proper medical intervention may lead to complications like pelvic inflammatory disease (PID). Remember, a healthcare professional’s guidance ensures accurate treatment and management of BV, improving your chances of a full recovery.
Don’t hesitate to seek professional medical advice. Early and accurate treatment of BV minimizes discomfort and the risk of long-term complications. Your health is important, and getting the right treatment is crucial.
- Amoxicillin and Bacterial Vaginosis: A Clarification
- Does Amoxicillin Treat Bacterial Vaginosis? Understanding the Ineffectiveness
- Why Amoxicillin Fails
- Recommended Treatment and Prevention
- Misconceptions about Amoxicillin Use for BV: Dispelling Common Myths
- Amoxicillin won’t cure BV.
- Resistance is a concern.
- Symptoms may persist even with correct treatment.
- Self-treating BV is dangerous.
- Over-the-counter remedies aren’t a substitute.
- Seeking Appropriate Treatment for Bacterial Vaginosis: Recommendations and Next Steps
- Confirming the Diagnosis
- Treatment Options
- Post-Treatment Care and Prevention
- Additional Resources
- Addressing Concerns
Amoxicillin and Bacterial Vaginosis: A Clarification
Amoxicillin is not a recommended treatment for bacterial vaginosis (BV).
BV is caused by an imbalance of bacteria in the vagina, and amoxicillin, a broad-spectrum antibiotic, targets a wider range of bacteria. While it might seem logical to use an antibiotic, treating BV with amoxicillin can disrupt the vaginal microbiome further, potentially worsening the condition or causing other infections. This inappropriate use could also contribute to antibiotic resistance.
Clinically proven treatments for BV include metronidazole or clindamycin, either as creams, gels, or oral medications. Your doctor will determine the most suitable option based on your specific situation. Self-treating BV is strongly discouraged.
Always consult a healthcare professional for diagnosis and treatment of BV. They can accurately identify the infection and prescribe the correct medication, minimizing potential complications and promoting a swift recovery.
Prompt medical attention ensures appropriate treatment and prevents potential long-term health issues associated with untreated or improperly treated BV.
Does Amoxicillin Treat Bacterial Vaginosis? Understanding the Ineffectiveness
No, amoxicillin is not effective for treating bacterial vaginosis (BV). Amoxicillin targets gram-positive bacteria, while BV is primarily caused by an imbalance of vaginal bacteria, often involving an overgrowth of Gardnerella vaginalis and other anaerobic bacteria.
Why Amoxicillin Fails
These anaerobic bacteria are not susceptible to amoxicillin. Using amoxicillin for BV won’t eliminate the causative organisms and may even disrupt the already fragile vaginal flora, potentially worsening symptoms or leading to further complications. Instead of amoxicillin, treatment focuses on antibiotics like metronidazole or clindamycin, specifically designed to target the bacteria responsible for BV.
Recommended Treatment and Prevention
If you suspect you have BV, see a healthcare professional for diagnosis and treatment. They can perform a pelvic exam and potentially a vaginal pH test to confirm the diagnosis and prescribe the appropriate medication. Metronidazole or clindamycin are commonly used, available in oral or topical forms. Maintaining good vaginal hygiene, avoiding douching, and practicing safe sex can help prevent future occurrences.
Misconceptions about Amoxicillin Use for BV: Dispelling Common Myths
Amoxicillin isn’t typically used to treat bacterial vaginosis (BV). Metronidazole or clindamycin are the preferred antibiotics. Using amoxicillin for BV is unlikely to be effective and could even lead to complications.
Amoxicillin won’t cure BV.
Many bacteria cause BV; amoxicillin’s effectiveness is limited against the specific bacteria responsible for this condition. Choosing the right antibiotic is key to successful treatment. Always consult your doctor for accurate diagnosis and treatment recommendations.
Resistance is a concern.
Misusing antibiotics promotes antibiotic resistance. This makes future infections harder to treat. Follow your doctor’s instructions carefully for any prescribed medication.
Symptoms may persist even with correct treatment.
BV symptoms can linger even after successful treatment. If symptoms don’t improve after completing the prescribed course of the *correct* antibiotic, consult your doctor for follow-up care. This isn’t a sign of treatment failure with a properly chosen antibiotic.
Self-treating BV is dangerous.
Never self-treat BV. Accurate diagnosis is critical. A healthcare professional can properly identify the cause of your symptoms and recommend the most appropriate treatment. Delaying proper treatment can lead to more severe complications. Seek professional medical advice for proper diagnosis and treatment.
Over-the-counter remedies aren’t a substitute.
Over-the-counter products might provide temporary relief from symptoms, but they won’t cure BV. They are not a replacement for antibiotic treatment prescribed by a doctor.
Seeking Appropriate Treatment for Bacterial Vaginosis: Recommendations and Next Steps
Bacterial vaginosis (BV) requires professional diagnosis and treatment. Don’t self-treat. Schedule an appointment with your gynecologist or another qualified healthcare provider.
Confirming the Diagnosis
Your doctor will perform a pelvic exam and may conduct a vaginal pH test or examine a sample of vaginal fluid under a microscope. These tests identify the bacteria causing BV and rule out other conditions.
Treatment Options
- Antibiotics: Metronidazole and clindamycin are common treatments. Your doctor will determine the best option and dosage based on your individual circumstances. Follow their instructions carefully, completing the entire course of medication, even if symptoms improve.
- Oral vs. Topical: Treatment may involve oral medication (pills) or topical application (creams or gels). Both are effective, but your doctor will advise on the most suitable method for you.
- Alternative Therapies: While antibiotics are the standard treatment, discuss any complementary therapies, such as probiotics, with your doctor. They can advise on their safety and effectiveness in your case.
Post-Treatment Care and Prevention
- Follow-up Appointment: Attend your follow-up appointment to ensure the infection is cleared.
- Hygiene Practices: Maintain good hygiene, avoiding douching, which can disrupt the natural vaginal balance.
- Sexual Practices: Discuss safe sex practices with your partner(s) to prevent reinfection.
- Recurring BV: If BV recurs frequently, further investigation may be necessary to identify any underlying factors contributing to the condition.
Additional Resources
The Centers for Disease Control and Prevention (CDC) and other reputable health organizations provide detailed information about BV. Consult these resources for more comprehensive details and support.
Addressing Concerns
If you experience any side effects from medication or have lingering concerns after treatment, contact your healthcare provider immediately. They’re there to answer your questions and provide ongoing support.