Doctors generally advise against Bactrim use while breastfeeding, especially during the first few weeks postpartum. This is due to the potential for sulfamethoxazole and trimethoprim, the active components of Bactrim, to pass into breast milk and possibly affect the infant.
However, if the benefits of Bactrim treatment outweigh the potential risks for the mother, careful monitoring of the infant is crucial. This includes close observation for any signs of allergic reactions, such as rash, diarrhea, or vomiting. Regular checkups with a pediatrician are also highly recommended to assess the baby’s health.
Lower doses of Bactrim are often preferred when breastfeeding to minimize exposure for the baby. Your doctor will carefully weigh the risks and benefits and may prescribe an alternative medication if possible. Discuss all your health concerns and medication history with your physician for personalized advice.
Remember: Never self-medicate while breastfeeding. Always consult your doctor or healthcare provider before taking any medication, including Bactrim, to ensure the safety of both you and your baby.
- Bactrim and Breastfeeding: A Comprehensive Guide
- Bactrim’s Presence in Breast Milk: Levels and Potential Risks
- Factors Affecting Bactrim Levels in Breast Milk
- Recommendations and Monitoring
- Further Considerations for Premature Infants
- Infant Sensitivity to Sulfamethoxazole and Trimethoprim: Monitoring for Side Effects
- Common Side Effects to Watch For
- Less Common but Serious Side Effects
- Reporting Side Effects
- Alternative Treatments During Breastfeeding: Exploring Safer Options
- When Bactrim is Necessary During Breastfeeding: Weighing Risks and Benefits
- Consulting Your Doctor: Importance of Personalized Advice
Bactrim and Breastfeeding: A Comprehensive Guide
Consult your doctor before taking Bactrim while breastfeeding. They can assess your individual needs and the risks versus benefits for both you and your baby.
Bactrim (sulfamethoxazole and trimethoprim) enters breast milk in small amounts. While generally considered safe, the level of drug transfer varies.
Factors influencing drug transfer include the mother’s dosage, the time since the last dose, and the baby’s metabolic rate.
Possible side effects in infants are rare but can include skin rashes or diarrhea. Monitoring your baby for these reactions is important.
Alternatives to Bactrim may be available, depending on your infection. Your doctor will discuss options if needed.
Proper hydration is crucial when taking Bactrim. This is especially important while breastfeeding to help flush out the medication and minimize potential side effects.
Always inform your healthcare provider about all medications you are taking, including over-the-counter drugs and supplements, before starting or continuing treatment with Bactrim during breastfeeding.
Remember: This information is for educational purposes only and does not constitute medical advice. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Bactrim’s Presence in Breast Milk: Levels and Potential Risks
Sulfamethoxazole and trimethoprim, the components of Bactrim, do transfer into breast milk. However, the levels are generally low, typically representing less than 1% of the maternal dose. This means your baby receives a minimal amount.
Factors Affecting Bactrim Levels in Breast Milk
- Dosage: Higher maternal doses result in slightly higher levels in breast milk.
- Drug formulation: Different formulations might exhibit minor variations in milk transfer.
- Mother’s metabolism: Individual variations in how the body processes Bactrim can slightly influence the amount transferred.
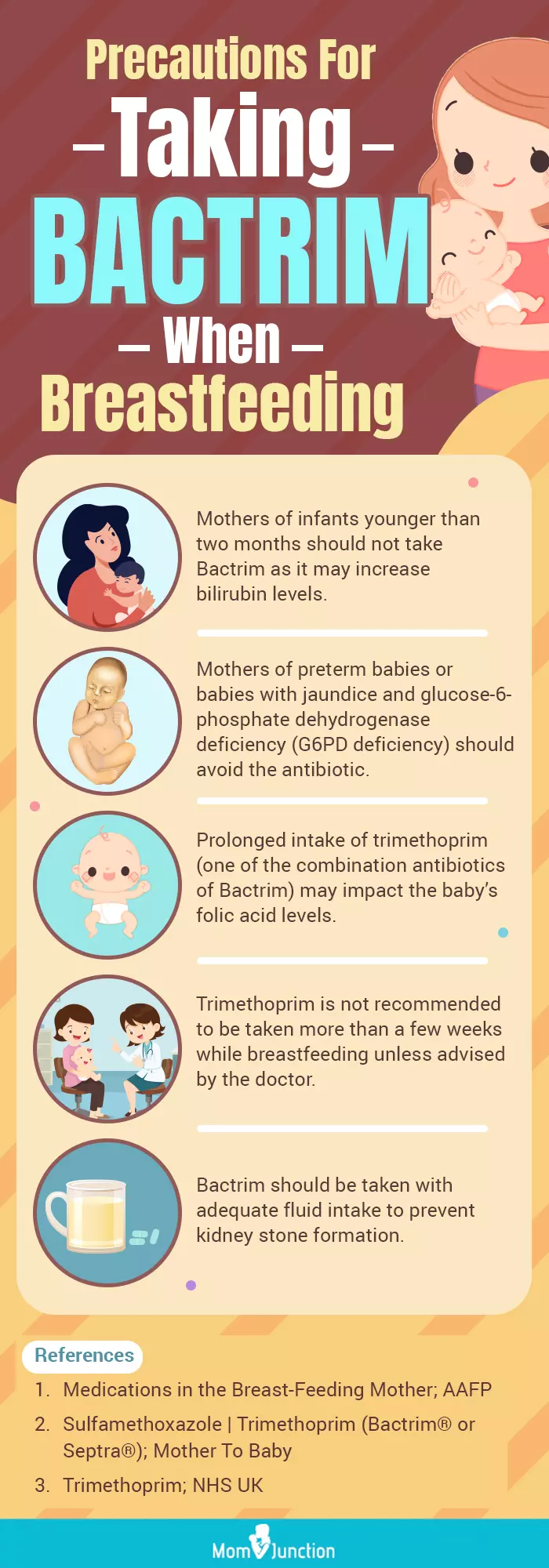
While the transferred amounts are usually insignificant, potential risks exist, particularly for newborns and premature infants. These risks are related to:
- Kernicterus: In rare cases, high levels of sulfamethoxazole can displace bilirubin from binding sites, potentially leading to kernicterus, especially in jaundiced newborns. Your doctor will consider this if your baby is jaundiced.
- Allergic reactions: Although uncommon, babies can develop allergic reactions to Bactrim through breast milk. Watch for signs like rash, diarrhea, or vomiting.
- Disruption of gut flora: The medication can affect the baby’s gut bacteria balance, although typically this is a minor concern.
Recommendations and Monitoring
- Discuss with your doctor: Before taking Bactrim while breastfeeding, always consult your healthcare provider. They can assess your individual risk and provide tailored advice.
- Monitor your baby: Closely observe your baby for any adverse reactions. Report any concerns immediately to your doctor.
- Alternative treatments: If possible, your doctor may suggest alternative antibiotics with lower risk to your breastfeeding infant.
Remember, the decision of whether or not to take Bactrim while breastfeeding should be made in conjunction with your doctor, considering the benefits of the medication against potential, albeit usually minor, risks to the infant.
Further Considerations for Premature Infants
Premature infants are especially vulnerable due to their immature liver and kidney function. Using Bactrim while breastfeeding a premature infant requires extra caution and careful monitoring, often prompting doctors to favor alternative treatment options.
Infant Sensitivity to Sulfamethoxazole and Trimethoprim: Monitoring for Side Effects
Closely monitor your baby for any unusual symptoms after you start taking Bactrim. This is particularly important during the first few days of treatment.
Common Side Effects to Watch For
- Rash: Look for any redness, bumps, or itching on your baby’s skin. Contact your doctor immediately if you see a rash.
- Jaundice: Notice any yellowing of the skin or whites of the eyes. This can indicate liver problems.
- Diarrhea: Increased frequency or changes in the consistency of your baby’s stools warrant attention. Severe or bloody diarrhea requires immediate medical attention.
- Vomiting: Persistent vomiting can indicate intolerance to the medication.
- Lethargy or Irritability: Unusual sleepiness or fussiness are potential signs of a problem.
- Poor feeding: Reduced interest in breastfeeding could signal discomfort or illness.
These symptoms can appear within a few days or weeks of starting Bactrim. Early detection is key.
Less Common but Serious Side Effects
- Anemia: Monitor your baby’s energy levels. Pale skin or unusual fatigue may indicate anemia.
- Crystalluria: This less common side effect involves kidney crystal formation and requires immediate medical attention. Signs might include changes in urination.
- Kernicterus: A rare but severe complication, particularly in premature babies. Symptoms include neurological issues like muscle weakness and problems with movement.
If you observe any of these side effects, contact your pediatrician immediately. They can assess the situation and advise you on the best course of action. Remember, prompt medical attention minimizes potential risks.
Reporting Side Effects
Your doctor may request regular follow-up appointments to monitor your baby’s condition while you are taking Bactrim. Thoroughly document and report any unusual symptoms to your pediatrician.
Alternative Treatments During Breastfeeding: Exploring Safer Options
Consider herbal remedies. Chamomile, for example, possesses anti-inflammatory properties and may offer relief from some infections, but always consult your doctor before using herbal remedies while breastfeeding. Dosage is critical.
Homeopathy might be another avenue. However, scientific evidence supporting its effectiveness remains limited. Discuss this with your healthcare provider to determine its suitability for your situation.
Proper hygiene practices significantly reduce infection risk. Thorough handwashing, safe food preparation, and avoiding exposure to sick individuals are key preventive measures.
Over-the-counter pain relievers, such as acetaminophen (Tylenol), can manage symptoms like fever and discomfort. Ibuprofen (Advil, Motrin) is generally considered safe, but always check with your doctor before use during breastfeeding.
Rest and hydration are underestimated. Prioritizing sleep and drinking plenty of fluids aids the body’s natural healing processes. Adequate rest supports milk production.
Remember: Always consult your doctor or a lactation consultant before starting any new treatment while breastfeeding. They can assess your specific needs and recommend the safest and most effective approach for you and your baby. They can help you weigh the risks and benefits of each option.
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for any health concerns or before making any decisions related to your health or treatment.
When Bactrim is Necessary During Breastfeeding: Weighing Risks and Benefits
Bactrim (sulfamethoxazole-trimethoprim) is sometimes necessary during breastfeeding to treat specific bacterial infections. Your doctor will carefully assess the severity of your infection against the potential risks to your baby.
Consider these factors: The type of infection significantly impacts the decision. A severe infection requiring immediate treatment often outweighs the low risk of Bactrim transferring to your baby through breast milk. Less serious infections might be managed with alternative therapies.
Your doctor will also consider your baby’s age and health. Premature babies or newborns with underlying health conditions may be at slightly higher risk from Bactrim exposure, necessitating a careful risk-benefit analysis.
| Factor | Impact on Decision |
|---|---|
| Infection Severity | Severe infections often necessitate Bactrim despite risks to infant. |
| Infant’s Age and Health | Premature or ill infants may require alternative treatments. |
| Alternative Treatments | Availability of safer alternatives influences treatment choice. |
| Duration of Treatment | Shorter treatment courses minimize infant exposure. |
The amount of Bactrim transferred through breast milk is generally low, and adverse effects in infants are rare. However, potential side effects in the infant, though uncommon, include allergic reactions, jaundice, and kernicterus (in rare cases). Your doctor will monitor both you and your baby closely.
Open communication with your healthcare provider is crucial. Discuss all concerns, including family history of allergies, before starting Bactrim. This collaborative approach ensures the best possible outcome for both you and your baby.
Consulting Your Doctor: Importance of Personalized Advice
Always discuss Bactrim use with your doctor before breastfeeding. Your doctor will consider your specific health situation, your baby’s age and health, and the severity of your infection.
They’ll weigh the potential benefits of Bactrim for you against any potential risks to your baby. This includes assessing the amount of medication that might transfer into your breast milk and its potential impact on your infant.
Factors like your baby’s weight, kidney function, and any pre-existing conditions will influence the doctor’s recommendation. Your individual medical history also plays a critical role in this decision.
Expect personalized guidance. This might involve adjusting your dosage, monitoring your baby’s health closely, or suggesting alternative treatments. Open communication with your doctor ensures you receive the safest and most effective care for both you and your baby.
Don’t hesitate to ask questions about potential side effects and monitoring strategies. A thorough discussion empowers you to make informed decisions about your health and your baby’s well-being.