Ciprofloxacin (Cipro) is generally not effective against MRSA (methicillin-resistant Staphylococcus aureus). MRSA strains possess a modified penicillin-binding protein, rendering them resistant to many antibiotics, including fluoroquinolones like Cipro. This resistance mechanism significantly impacts treatment options.
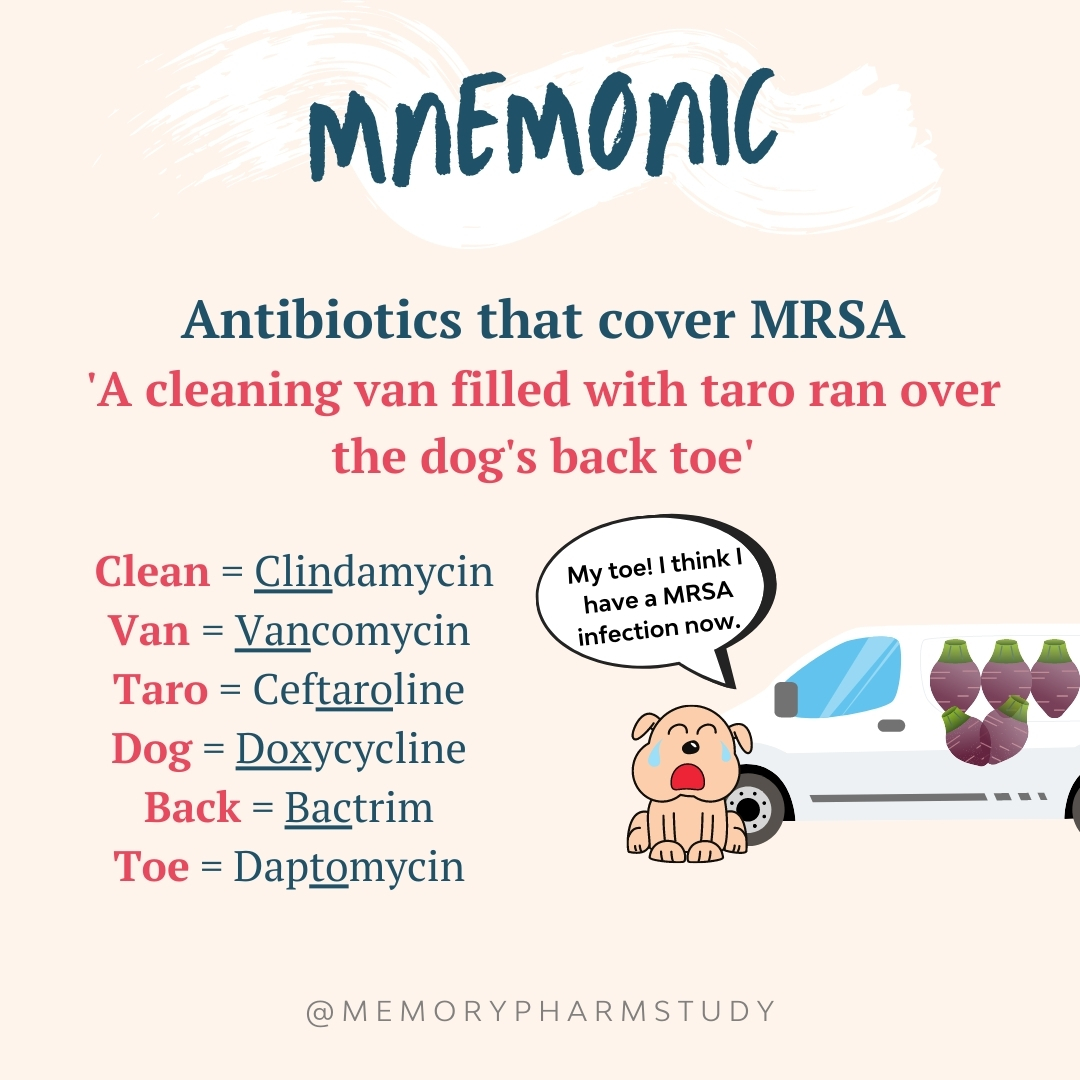
Alternative antibiotics, such as vancomycin, linezolid, daptomycin, or ceftaroline, usually provide better coverage for MRSA infections. The specific choice depends on factors like infection site, patient history, and local antibiotic susceptibility patterns. Your physician will consider these factors to determine the optimal treatment plan.
Always consult a healthcare professional for diagnosis and treatment of MRSA or any suspected bacterial infection. Self-treating can be dangerous and may lead to treatment failure and the development of further antibiotic resistance. Relying on outdated or inaccurate information regarding antibiotic efficacy can have serious health consequences.
Current guidelines strongly recommend against using Cipro for MRSA infections due to its low effectiveness and the potential for promoting antibiotic resistance. Proper antibiotic stewardship practices are paramount in managing bacterial infections and minimizing the development of resistance.
- Ciprofloxacin Coverage for MRSA: A Detailed Overview
- MRSA Infection: A Brief Overview of the Bacteria and its Resistance
- Understanding MRSA Resistance Mechanisms
- Ciprofloxacin Mechanism of Action: How it Typically Works
- Targeting Bacterial Enzymes
- Consequences of Inhibition
- Ciprofloxacin’s Susceptibility to MRSA: Understanding the Limitations
- Resistance Mechanisms
- Treatment Implications
- Alternative Treatment Strategies
- Factors Influencing Ciprofloxacin Effectiveness Against MRSA
- Alternative Antibiotics for MRSA Treatment: Exploring Effective Options
- When Ciprofloxacin Might Be Considered in MRSA Infection (Rare Cases)
- Specific Scenarios
- Important Considerations
- Disclaimer
- Importance of Culture and Sensitivity Testing in MRSA Treatment Decisions
Ciprofloxacin Coverage for MRSA: A Detailed Overview
Ciprofloxacin generally lacks effectiveness against MRSA (methicillin-resistant Staphylococcus aureus).
MRSA strains exhibit resistance mechanisms that render ciprofloxacin largely ineffective. These mechanisms include mutations in the bacterial DNA gyrase and topoisomerase IV enzymes, the targets of ciprofloxacin.
- Susceptibility Testing is Crucial: Always perform susceptibility testing to determine the antibiotic susceptibility profile of the specific MRSA isolate. This is paramount for guiding treatment decisions.
- Alternative Antibiotics: Effective treatment options for MRSA infections include:
- Vancomycin
- Daptomycin
- Linezolid
- Ceftaroline
- Telavancin
The choice depends on factors like the infection site, severity, and patient’s medical history. Consult your local antibiogram for the most effective options in your region.
- Combination Therapy: In severe cases, combination therapy with multiple antibiotics might be considered. This approach should be guided by expert consultation and local guidelines.
- Infection Control: Strict adherence to infection control protocols is vital in preventing MRSA spread. This includes proper hand hygiene, contact precautions, and environmental disinfection.
Specific clinical situations may justify using ciprofloxacin despite its generally poor efficacy against MRSA. However, this should only be considered in the context of comprehensive evaluation by an infectious disease specialist, local susceptibility data, and an informed understanding of the risks and benefits.
- Rare Exceptions: In some rare instances, a specific MRSA strain might exhibit susceptibility to ciprofloxacin. This is exceptionally uncommon and necessitates confirmation through susceptibility testing.
- Empirical Treatment: Ciprofloxacin may sometimes be considered as part of initial empirical treatment for infections in settings where MRSA is unlikely and rapid diagnostic results are unavailable. However, this is a strategy with limited applicability and necessitates prompt reassessment based on culture and susceptibility results.
Remember, appropriate antibiotic stewardship is crucial in combating antibiotic resistance. Using antibiotics judiciously and only when clinically indicated is paramount. Always consult current clinical guidelines and consult with specialists to provide the best possible care.
MRSA Infection: A Brief Overview of the Bacteria and its Resistance
Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterium causing skin infections, ranging from minor boils to severe pneumonia and bloodstream infections. Its resistance stems from a modified penicillin-binding protein (PBP2a), preventing common antibiotics like methicillin from binding and killing the bacteria. This resistance mechanism makes treating MRSA infections challenging, requiring stronger antibiotics.
Understanding MRSA Resistance Mechanisms
MRSA’s resistance isn’t limited to methicillin. Many strains exhibit resistance to multiple antibiotic classes, including tetracyclines, aminoglycosides, and fluoroquinolones. This multi-drug resistance arises through various genetic mechanisms like mutations, gene transfer, and acquisition of resistance genes. The spread of MRSA, particularly in healthcare settings, accelerates the evolution of increasingly resistant strains.
Proper infection control practices, including meticulous hand hygiene and appropriate isolation procedures, remain critical in preventing the spread of MRSA and minimizing the development of further antibiotic resistance. Accurate diagnosis, prompt treatment with appropriate antibiotics (guided by susceptibility testing), and close monitoring of patients are crucial for successful outcomes.
Ciprofloxacin Mechanism of Action: How it Typically Works
Ciprofloxacin targets bacterial DNA gyrase and topoisomerase IV. These enzymes are crucial for bacterial DNA replication, transcription, and repair. Ciprofloxacin inhibits these enzymes by binding to them, preventing DNA unwinding and replication. This halts bacterial growth and ultimately leads to cell death.
Targeting Bacterial Enzymes
Specifically, ciprofloxacin interacts with the A subunit of DNA gyrase and topoisomerase IV. This interaction prevents the enzymes from properly functioning. The precise mechanism involves blocking the enzymes’ ability to change DNA supercoiling. This process is fundamentally important for DNA replication and repair in bacteria. The result is a disruption of bacterial DNA metabolism and subsequent bacterial cell death.
Consequences of Inhibition
The inhibition of these enzymes results in DNA damage and fragmentation. This damage prevents the bacteria from reproducing and ultimately kills them. It’s worth remembering that this mechanism is specific to bacterial enzymes; human cells lack these specific targets, reducing the likelihood of significant human toxicity.
Ciprofloxacin’s Susceptibility to MRSA: Understanding the Limitations
Ciprofloxacin rarely treats MRSA infections. MRSA bacteria developed resistance mechanisms against fluoroquinolones, the antibiotic class to which ciprofloxacin belongs. This resistance renders ciprofloxacin ineffective in most cases.
Resistance Mechanisms
MRSA’s resistance stems primarily from mutations in the genes encoding topoisomerase IV and DNA gyrase, the enzymes ciprofloxacin targets. These mutations prevent the drug from binding and inhibiting bacterial DNA replication.
Treatment Implications
Clinicians should avoid prescribing ciprofloxacin for suspected or confirmed MRSA infections. Other antibiotic classes, such as glycopeptides (vancomycin, teicoplanin) or lipopeptides (daptomycin), often demonstrate better efficacy. Always conduct susceptibility testing to guide antibiotic selection. Treatment decisions require considering patient factors, infection severity, and local resistance patterns.
Alternative Treatment Strategies
Effective MRSA treatment requires a tailored approach. Options include intravenous vancomycin, linezolid, daptomycin, or ceftaroline. Surgical debridement might be necessary for severe infections, especially those involving abscesses or necrotic tissue. Close monitoring of treatment response is crucial.
Factors Influencing Ciprofloxacin Effectiveness Against MRSA
Ciprofloxacin’s success against MRSA hinges on several key factors. Understanding these helps predict treatment outcomes.
- MRSA Strain Susceptibility: Not all MRSA strains are equally susceptible. Laboratory testing determines minimum inhibitory concentrations (MICs), providing a crucial measure of susceptibility. High MIC values indicate reduced efficacy.
- Patient-Specific Factors: Individual differences matter significantly. Kidney and liver function influence drug metabolism and clearance. Age impacts drug distribution and elimination. Underlying health conditions can affect response.
- Drug Concentration: Achieving therapeutic drug levels at the infection site is paramount. Dosage, frequency of administration, and route of administration (oral vs. intravenous) all influence achievable concentrations. Inadequate drug levels promote resistance development.
- Site of Infection: Ciprofloxacin’s penetration into various tissues differs. Deep-seated infections, like bone or joint infections, might not reach sufficient concentrations for eradication even with appropriate dosing.
- Duration of Treatment: Shortening treatment duration increases the risk of treatment failure and relapse. Guidelines suggest longer treatment courses for severe infections or those with poor initial responses. Adherence to the prescribed regimen is also critical.
- Combination Therapy: Combining ciprofloxacin with other antibiotics may enhance its effect against MRSA, especially in cases of high MICs. This approach can help overcome resistance mechanisms.
Proper antibiotic stewardship is key. Empirical use without prior susceptibility testing risks treatment failure and contributes to resistance development. Close monitoring of clinical response is always necessary.
- Regular clinical assessments are needed to monitor improvement.
- If no response is seen within 48-72 hours, reconsider treatment.
- Consider alternative antibiotics guided by culture and sensitivity testing.
Alternative Antibiotics for MRSA Treatment: Exploring Effective Options
Daptomycin is a potent option for treating serious MRSA infections. It works differently than many other antibiotics, directly disrupting bacterial cell membranes.
Linezolid is another powerful choice, particularly for skin and soft tissue infections caused by MRSA. It inhibits bacterial protein synthesis, effectively stopping their growth.
Tigecycline offers broad-spectrum coverage, including MRSA, and can be useful when other antibiotics fail. However, it’s crucial to note its potential for side effects.
Ceftolozane-tazobactam demonstrates efficacy against some MRSA strains, primarily those with specific resistance profiles. Always check susceptibility testing before prescribing.
Choosing the right antibiotic depends on various factors. Consider the specific MRSA strain, the infection site, and patient-specific factors like allergies and kidney function.
| Antibiotic | Mechanism of Action | Typical Use | Important Note |
|---|---|---|---|
| Daptomycin | Membrane disruption | Serious MRSA infections | Monitor creatine kinase levels |
| Linezolid | Protein synthesis inhibition | Skin and soft tissue infections | Potential for myelosuppression |
| Tigecycline | Protein synthesis inhibition | Broad-spectrum, including MRSA | Potential for side effects |
| Ceftolozane-tazobactam | Beta-lactam/beta-lactamase inhibitor | Specific MRSA strains | Susceptibility testing required |
Always consult current treatment guidelines and local antibiograms to guide your choices. Close monitoring of the patient’s response to therapy is paramount.
When Ciprofloxacin Might Be Considered in MRSA Infection (Rare Cases)
Ciprofloxacin, a fluoroquinolone antibiotic, generally lacks effectiveness against MRSA. However, very rare instances exist where its use might be considered. This is primarily in situations where other, more effective antibiotics are contraindicated or have failed.
Specific Scenarios
Susceptibility Testing: The only justification for using ciprofloxacin against MRSA is if in vitro susceptibility testing demonstrates sensitivity. This testing should be performed before initiating treatment, not after failure of other agents. Expect this to be exceptionally rare.
Treatment Failure with Multiple Antibiotics: If a patient has experienced treatment failure with multiple recommended antibiotics for MRSA, and ciprofloxacin demonstrates in vitro susceptibility, a physician might consider it as a last resort. This decision hinges on a careful risk-benefit assessment, weighing the potential benefits against the known limitations of ciprofloxacin and the risk of developing further antibiotic resistance.
Important Considerations
Resistance Concerns: Using ciprofloxacin against MRSA significantly increases the risk of developing resistance to this antibiotic class. This has broad implications for the treatment of other bacterial infections. This outcome should be carefully considered.
Alternative Treatments: Always prioritize established effective MRSA treatments like daptomycin, vancomycin, linezolid, or ceftaroline before considering ciprofloxacin. Thorough investigation and adherence to updated guidelines are crucial for selecting the appropriate treatment.
Disclaimer
This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for diagnosis and treatment of MRSA or any infection.
Importance of Culture and Sensitivity Testing in MRSA Treatment Decisions
Always perform culture and sensitivity testing before initiating MRSA treatment. This crucial step guides antibiotic selection, ensuring optimal efficacy and minimizing resistance development.
A positive MRSA culture confirms the infection’s presence. Sensitivity testing, or antibiogram, then determines which antibiotics effectively inhibit the specific strain’s growth. This information directly impacts treatment choice; Ciprofloxacin, for example, may or may not be effective depending on the strain’s susceptibility profile.
Ignoring these tests risks prescribing ineffective antibiotics, prolonging illness, and increasing the likelihood of antibiotic resistance. A targeted approach, informed by testing, improves patient outcomes and conserves antibiotic resources.
The antibiogram provides a Minimum Inhibitory Concentration (MIC) value for each tested antibiotic. Lower MIC values indicate greater susceptibility, suggesting a higher probability of successful treatment. Clinicians use this data alongside patient-specific factors to choose the most appropriate antibiotic.
Prompt results from culture and sensitivity tests are paramount. Delayed results can delay appropriate treatment, potentially leading to worse outcomes. Prioritize rapid testing methods when feasible.
Remember, empirical therapy, started before results are available, should only be a temporary measure. Adjust antibiotic therapy based on the culture and sensitivity results as soon as they are available. This approach optimizes treatment and helps combat antimicrobial resistance.