Ciprofloxacin and penicillin target different bacterial infections. Penicillin, a beta-lactam antibiotic, excels against gram-positive bacteria like those causing strep throat and pneumonia. Ciprofloxacin, a fluoroquinolone, effectively combats gram-negative bacteria responsible for urinary tract infections and some types of pneumonia. Your doctor determines the best choice based on your specific infection.
Consider the severity and location of your infection. For instance, penicillin remains the first-line treatment for many uncomplicated bacterial skin infections. However, ciprofloxacin’s broader spectrum makes it suitable for treating more resistant infections, especially those affecting the urinary tract or respiratory system. Always consult a healthcare professional for diagnosis and treatment recommendations.
Side effects differ. Penicillin allergies are common, ranging from mild rashes to severe anaphylaxis. Ciprofloxacin, while generally well-tolerated, can cause gastrointestinal upset, tendonitis, or rarely, nerve damage. Open communication with your doctor about your medical history and any potential drug interactions is paramount. This ensures the safest and most effective treatment plan.
Remember: Never self-medicate. Antibiotic resistance is a growing concern, and inappropriate antibiotic use exacerbates this problem. Always follow your doctor’s prescribed dosage and duration to ensure complete eradication of the infection and to prevent the development of resistant bacteria.
- Ciprofloxacin vs. Penicillin: A Detailed Comparison
- Spectrum of Activity: Which Bacteria Do They Target?
- Ciprofloxacin Targets:
- Penicillin Targets:
- Mechanism of Action: How Do They Kill Bacteria?
- Ciprofloxacin’s Target: DNA Replication
- Penicillin’s Mechanism: Cell Wall Synthesis Inhibition
- Comparison Table
- Common Uses: When is Each Antibiotic Prescribed?
- Side Effects and Potential Risks: Comparing Adverse Reactions
- Ciprofloxacin Side Effects
- Making Informed Decisions
- Choosing the Right Antibiotic: Considerations for Doctors and Patients
- Patient-Specific Factors
- Antibiotic Properties
- Resistance and Stewardship
- Seeking Medical Advice
Ciprofloxacin vs. Penicillin: A Detailed Comparison
Choose Ciprofloxacin for infections caused by gram-negative bacteria like E. coli and Pseudomonas aeruginosa; penicillin excels against gram-positive bacteria such as Streptococcus and Staphylococcus (excluding penicillin-resistant strains).
Mechanism of Action: Ciprofloxacin, a fluoroquinolone, inhibits bacterial DNA replication. Penicillin, a beta-lactam antibiotic, interferes with bacterial cell wall synthesis.
Spectrum of Activity: Ciprofloxacin possesses a broader spectrum, targeting both gram-positive and gram-negative bacteria, although its activity against gram-positive bacteria is generally weaker than penicillin’s. Penicillin’s spectrum is narrower, primarily focusing on gram-positive bacteria.
Adverse Effects: Ciprofloxacin can cause tendonitis and rupture, particularly in older adults. Penicillin commonly leads to allergic reactions, ranging from mild rashes to severe anaphylaxis. Gastrointestinal upset is possible with both antibiotics.
Resistance: Resistance to both Ciprofloxacin and penicillin is a growing concern. Overuse contributes significantly to the development of resistant strains. Appropriate antibiotic stewardship is paramount.
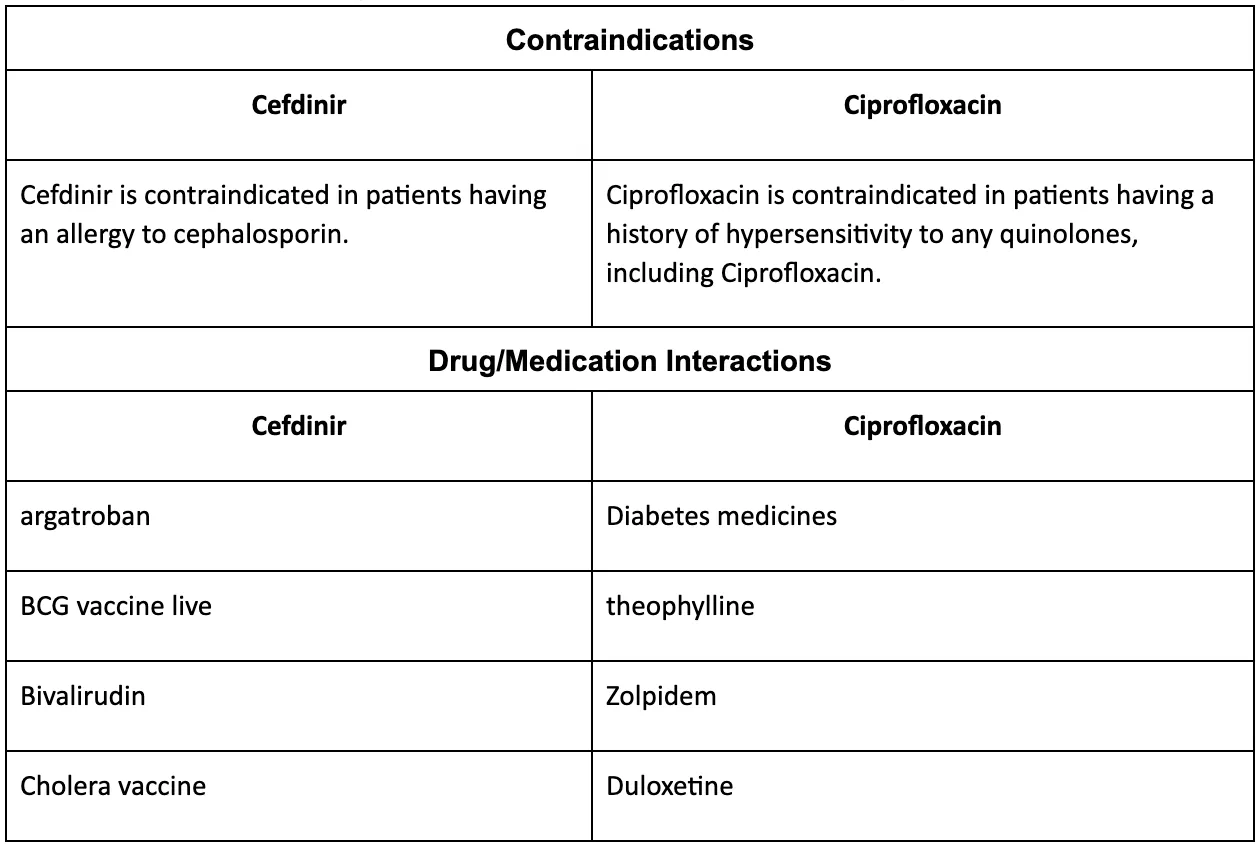
Drug Interactions: Ciprofloxacin interacts with several medications, including antacids and theophylline. Penicillin may interact with certain drugs that affect kidney function.
Administration: Both antibiotics are available in various formulations, including oral and intravenous. Dosage and duration of treatment depend on the specific infection and patient factors. Always follow your doctor’s instructions.
Note: This information is for educational purposes only and does not substitute professional medical advice. Always consult a healthcare provider for diagnosis and treatment of infections.
Spectrum of Activity: Which Bacteria Do They Target?
Ciprofloxacin and penicillin target different types of bacteria. Ciprofloxacin, a fluoroquinolone, excels against Gram-negative bacteria, while penicillin, a beta-lactam antibiotic, primarily works against Gram-positive bacteria. This difference stems from their distinct mechanisms of action and bacterial cell wall structures.
Ciprofloxacin Targets:
- Enterobacteriaceae (E. coli, Salmonella, Shigella): Ciprofloxacin effectively combats many infections caused by these common intestinal bacteria.
- Pseudomonas aeruginosa: A particularly problematic bacterium in hospital settings, ciprofloxacin is often a treatment option.
- Haemophilus influenzae: A cause of respiratory infections, this bacteria is susceptible to ciprofloxacin.
- Some Gram-positive bacteria: While primarily targeting Gram-negative bacteria, ciprofloxacin demonstrates activity against certain Gram-positive species, although often less effectively than penicillin.
Penicillin Targets:
- Streptococcus pneumoniae: A major cause of pneumonia and other respiratory infections, penicillin remains a vital treatment.
- Streptococcus pyogenes (Group A Streptococcus): Responsible for strep throat and other serious infections, penicillin is often the first-line treatment.
- Staphylococcus aureus (some strains): Penicillin remains effective against certain strains of S. aureus, though antibiotic resistance is a growing concern.
- Neisseria meningitidis: A cause of bacterial meningitis, penicillin is commonly used in treatment.
- Treponema pallidum (syphilis): Penicillin is the standard treatment for syphilis.
Note: Antibiotic resistance is an ongoing challenge. Always consult a healthcare professional for accurate diagnosis and appropriate antibiotic selection. The effectiveness of each antibiotic can vary based on bacterial species, infection location, and patient factors. These lists are not exhaustive; many other bacteria are susceptible to either ciprofloxacin or penicillin.
Mechanism of Action: How Do They Kill Bacteria?
Ciprofloxacin and penicillin target bacteria using completely different methods. Ciprofloxacin, a fluoroquinolone, inhibits bacterial DNA gyrase and topoisomerase IV. These enzymes are crucial for DNA replication and cell division. By blocking these enzymes, ciprofloxacin prevents bacteria from replicating their genetic material, ultimately leading to their death.
Ciprofloxacin’s Target: DNA Replication
Specifically, ciprofloxacin binds to these enzymes, interfering with their ability to unwind and supercoil DNA. This process is necessary for both bacterial replication and repair. Without this ability, the bacteria cannot copy their DNA or fix any damage, hindering their survival.
Penicillin’s Mechanism: Cell Wall Synthesis Inhibition
Penicillin, a beta-lactam antibiotic, works by targeting bacterial cell wall synthesis. It inhibits the enzyme transpeptidase, which is responsible for building peptidoglycan, a crucial component of the bacterial cell wall. Without proper peptidoglycan, the bacterial cell wall becomes weak and unstable.
This weakening leads to cell lysis, or rupture, effectively killing the bacteria. Different penicillins have varying levels of effectiveness against different types of bacteria, due to variations in bacterial cell wall structures and transpeptidase enzyme variations.
Comparison Table
| Antibiotic | Mechanism of Action | Target Enzyme | Bacterial Effect |
|---|---|---|---|
| Ciprofloxacin | Inhibition of DNA gyrase and topoisomerase IV | DNA Gyrase, Topoisomerase IV | Prevents DNA replication and repair |
| Penicillin | Inhibition of transpeptidase | Transpeptidase | Weakens cell wall, causing lysis |
Common Uses: When is Each Antibiotic Prescribed?
Ciprofloxacin, a fluoroquinolone antibiotic, effectively treats various bacterial infections, including urinary tract infections (UTIs), respiratory tract infections like bronchitis and pneumonia (certain types), and skin infections. Doctors also prescribe it for infections related to bone, joints, and gastrointestinal issues, particularly those caused by susceptible bacteria. It’s also used in treating some sexually transmitted infections (STIs).
Penicillin, a beta-lactam antibiotic, is a cornerstone in treating infections caused by susceptible bacteria. Common uses include strep throat, pneumonia (certain types), some skin infections, and syphilis. Penicillin remains a vital choice for treating bacterial endocarditis and certain bacterial meningitides. Many penicillin variations exist, each targeting specific bacteria.
The choice between ciprofloxacin and penicillin hinges on the specific infection, the bacteria causing it, and the patient’s medical history. Penicillin’s many forms provide options for various sensitivities, while ciprofloxacin’s broader activity makes it suitable for certain situations where other antibiotics are less effective. A healthcare professional must determine the appropriate antibiotic based on lab results and patient-specific factors.
Side Effects and Potential Risks: Comparing Adverse Reactions
Ciprofloxacin and penicillin, while both antibiotics, carry different side effect profiles. Penicillin allergies are a significant concern; reactions range from mild rashes to life-threatening anaphylaxis. Always inform your doctor of any prior allergic reactions before taking penicillin. Common side effects include nausea, vomiting, and diarrhea. Less frequent but possible issues include yeast infections and seizures.
Ciprofloxacin Side Effects
Ciprofloxacin, a fluoroquinolone, presents a distinct side effect profile. Tendonitis and tendon rupture are serious risks, particularly for older adults or those taking corticosteroids. Peripheral neuropathy, characterized by numbness, tingling, and pain in the extremities, is another potential adverse event. Gastrointestinal issues like nausea and diarrhea are also common. Less frequently, ciprofloxacin can affect the central nervous system, potentially causing dizziness, confusion, or seizures. Furthermore, photosensitivity, increasing sun sensitivity, may occur. Always discuss potential risks and alternative treatments with your physician before starting any antibiotic course.
Making Informed Decisions
This information is for general knowledge only; it does not substitute professional medical advice. Always consult your doctor to determine the best antibiotic for your specific condition and to discuss the potential benefits and risks related to your individual health status and other medications you may be taking. They can assess your medical history and allergies to make the safest and most effective treatment choice.
Choosing the Right Antibiotic: Considerations for Doctors and Patients
Always prioritize identifying the specific bacteria causing the infection through laboratory testing. This guides antibiotic selection for optimal treatment and minimizes the risk of antibiotic resistance.
Patient-Specific Factors
Doctors must account for patient allergies, previous antibiotic use, kidney or liver function, pregnancy status, and potential drug interactions. A patient’s age also influences antibiotic choice; infants and the elderly may require different dosages or antibiotics altogether. Discuss all medications – including over-the-counter drugs and supplements – with your doctor. This aids in preventing potentially harmful interactions.
Antibiotic Properties
Ciprofloxacin targets a broader range of bacteria than penicillin. However, penicillin remains highly effective against specific infections, particularly those caused by gram-positive bacteria. The site of infection influences antibiotic choice; some antibiotics reach certain tissues better than others. Consider the antibiotic’s half-life – how long it remains active in the body – to determine appropriate dosing frequency. Side effects vary significantly between antibiotics; discuss these with your doctor to make an informed decision.
Resistance and Stewardship
Antibiotic resistance is a serious global health threat. Therefore, responsible antibiotic use is paramount. Doctors must prescribe only when necessary, selecting the narrowest-spectrum antibiotic effective against the identified bacteria. Patients should complete their prescribed course of antibiotics, even if they feel better sooner. This prevents incomplete treatment and reduces the risk of resistance development. Discuss antibiotic stewardship programs with your doctor or pharmacist to learn how you can contribute to responsible antibiotic use.
Seeking Medical Advice
Self-treating bacterial infections is dangerous and can lead to severe complications and antibiotic resistance. Consult a healthcare professional for diagnosis and treatment. They will conduct a proper evaluation, order the necessary tests, and select the most appropriate antibiotic for your specific needs. Active collaboration between doctor and patient ensures optimal outcomes.