Need to understand the combined use of gentamicin and lasix? Focus on monitoring kidney function. Regular blood tests, specifically creatinine and BUN levels, are critical for detecting potential nephrotoxicity. Adjust dosages based on these results; close monitoring prevents complications.
Lasix, a potent diuretic, increases gentamicin’s concentration in the kidneys, raising the risk of renal damage. Therefore, precise dosage adjustments are paramount. Consult the latest prescribing information for both medications for detailed guidelines on safe administration and monitoring protocols.
Hydration is key. Encourage adequate fluid intake to help flush out gentamicin and reduce its concentration in the kidneys. This simple measure, alongside careful lab monitoring, significantly decreases the chances of adverse effects.
Remember: This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for personalized treatment plans and medication management. They can assess individual patient needs and adjust the treatment accordingly, ensuring safety and efficacy.
Always prioritize patient safety and follow established clinical guidelines. Regular communication with the medical team facilitates optimal patient outcomes when using this drug combination.
- Gentamicin and Lasix: A Detailed Overview
- Gentamicin and Lasix: Combined Use in Treating Severe Infections with Fluid Retention
- Monitoring Vital Signs and Renal Function
- Dosage and Administration Considerations
- Potential Drug Interactions and Adverse Effects of Gentamicin and Lasix Combination
- Monitoring and Management of Patients Receiving Gentamicin and Lasix
- Monitoring for Ototoxicity
- Managing Electrolyte Imbalances
- Fluid Balance Assessment
- Other Important Considerations:
- Specific Lab Monitoring Schedule:
Gentamicin and Lasix: A Detailed Overview
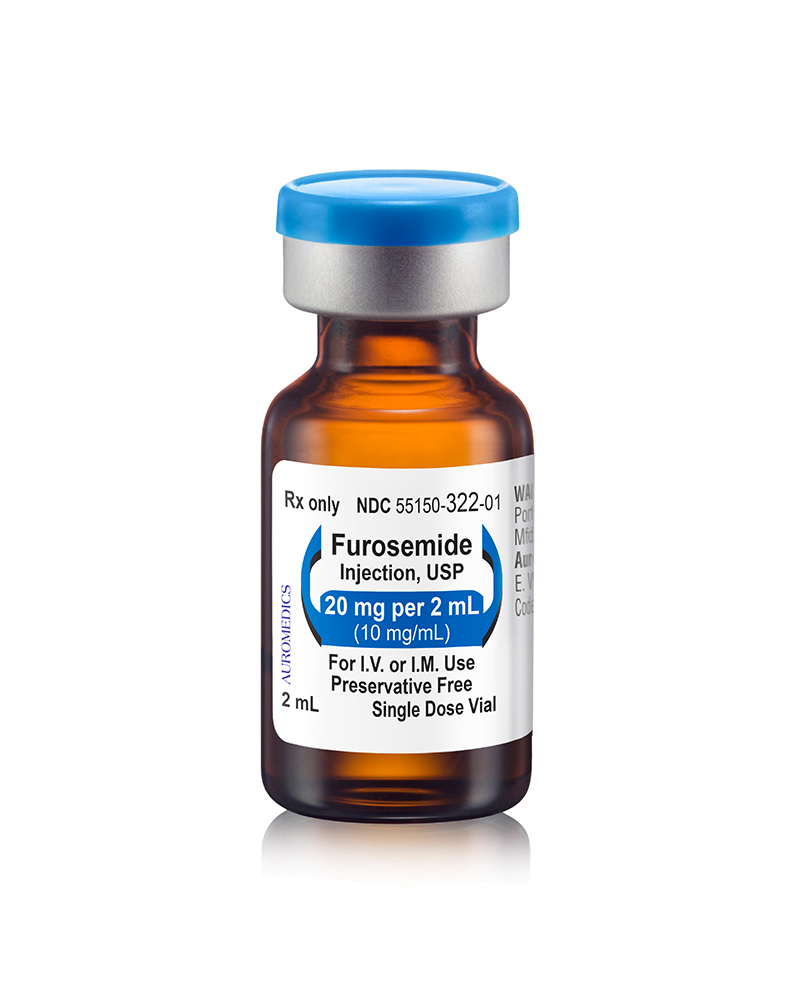
Gentamicin, an aminoglycoside antibiotic, and Lasix (furosemide), a loop diuretic, are frequently used in hospital settings, often concurrently. However, their combined use necessitates careful monitoring.
Gentamicin’s nephrotoxicity is a significant concern. Lasix, by increasing urine output, can exacerbate this risk, potentially leading to acute kidney injury. Regular monitoring of serum creatinine and glomerular filtration rate (GFR) is critical. Consider adjusting gentamicin dosage based on renal function tests, potentially reducing the frequency or amount administered.
Ototoxicity is another adverse effect of gentamicin. While Lasix doesn’t directly cause ototoxicity, prolonged use and dehydration (a possible side effect of Lasix) can worsen gentamicin-induced hearing loss. Regular audiometric testing may be warranted, particularly in patients with pre-existing hearing problems.
Electrolyte imbalances are common with Lasix, causing hypokalemia, hypomagnesemia, and hyponatremia. Gentamicin can further contribute to these imbalances. Closely monitor serum electrolyte levels and adjust accordingly with potassium or magnesium supplementation as needed.
Hydration is paramount. Adequate fluid intake helps mitigate the nephrotoxicity of gentamicin and the dehydration risks associated with Lasix. Intravenous fluids may be necessary, particularly in patients with reduced oral intake.
Alternative medications should be considered if possible. If the clinical picture allows, explore alternative antibiotics with less nephrotoxic potential and diuretics with a different mechanism of action.
This information is for educational purposes only and should not be considered medical advice. Always consult a healthcare professional for personalized treatment plans.
Gentamicin and Lasix: Combined Use in Treating Severe Infections with Fluid Retention
This combination therapy addresses two distinct but often co-occurring problems: severe infection and fluid overload. Gentamicin, an aminoglycoside antibiotic, combats serious bacterial infections. Lasix, a potent diuretic, efficiently removes excess fluid from the body. Their simultaneous use is clinically relevant in conditions where both infection and fluid retention are present, such as severe sepsis or heart failure complicated by infection.
Monitoring Vital Signs and Renal Function
Close monitoring of vital signs, including blood pressure and heart rate, is crucial during combined Gentamicin and Lasix therapy. Regular assessment of renal function, through serum creatinine and blood urea nitrogen (BUN) levels, is also necessary. Gentamicin is nephrotoxic, and Lasix can further impair kidney function, particularly in patients with pre-existing renal issues. Adjusting dosages based on these lab results is frequently required. Electrolyte imbalances, especially hypokalemia, are possible side effects requiring careful management through supplementation when indicated.
Dosage and Administration Considerations
Dosage adjustments depend heavily on individual patient factors including age, weight, kidney function, and the severity of both the infection and fluid retention. A physician will determine the appropriate dosage of each drug. Gentamicin is usually administered intravenously or intramuscularly, while Lasix is administered intravenously or orally. The frequency of administration differs based on individual needs and must be carefully planned.
Potential Drug Interactions and Adverse Effects of Gentamicin and Lasix Combination
Combining gentamicin and lasix increases the risk of nephrotoxicity. Gentamicin, an aminoglycoside antibiotic, is already known to damage the kidneys. Lasix, a potent diuretic, further reduces blood flow to the kidneys, exacerbating this risk. Monitor kidney function closely with serum creatinine and blood urea nitrogen (BUN) levels. Frequent monitoring is crucial, especially in patients with pre-existing kidney disease or the elderly.
Ototoxicity, or hearing damage, is another concern. Gentamicin’s ototoxic effects are amplified by dehydration induced by Lasix. Regular hearing tests may be necessary, especially during prolonged treatment. Report any dizziness, tinnitus (ringing in the ears), or hearing loss immediately.
Electrolyte imbalances are common with Lasix. Hypokalaemia (low potassium) is a significant risk, potentially worsened by gentamicin. Regular electrolyte monitoring is vital. Potassium supplementation may be required. Careful hydration is also necessary to minimize electrolyte disturbances.
Patients should be advised to report any signs of kidney problems (reduced urine output, swelling, fatigue) or hearing changes promptly. Adjusting dosages or selecting alternative medications may be necessary in cases of severe adverse effects or pre-existing conditions limiting renal or auditory function. Always consult with a healthcare professional before combining these drugs or making any medication changes.
Remember: This information is for educational purposes and does not substitute professional medical advice. Individual patient response varies, and a healthcare provider should tailor treatment to specific patient needs.
Monitoring and Management of Patients Receiving Gentamicin and Lasix
Closely monitor renal function. Obtain baseline serum creatinine and creatinine clearance before initiating therapy, then repeat these measurements every 2-3 days during treatment. Adjust dosages based on these results. Consider using estimated glomerular filtration rate (eGFR) calculations for a more comprehensive assessment of renal function.
Monitoring for Ototoxicity
Gentamicin can cause ototoxicity. Monitor for hearing loss, tinnitus, and vertigo. Regular audiometry testing, especially in patients at higher risk (e.g., those with pre-existing hearing impairment or renal dysfunction), is recommended. Discontinue gentamicin if significant hearing loss occurs.
Managing Electrolyte Imbalances
Lasix (furosemide) is a potent diuretic that can induce hypokalemia, hyponatremia, and hypomagnesemia. Regularly monitor serum electrolytes, particularly potassium, sodium, and magnesium levels. Potassium supplementation might be needed. Closely observe patients for signs and symptoms of electrolyte imbalance, such as muscle weakness, arrhythmias, and confusion.
Fluid Balance Assessment
Monitor daily weight, fluid intake and output, and urine output. This helps assess fluid status and effectiveness of the diuretic. Adjust Lasix dosage accordingly to achieve the desired diuretic effect without causing excessive dehydration.
Other Important Considerations:
- Regularly assess blood pressure, noting any significant changes.
- Monitor for signs of dehydration, including decreased urine output, dry mucous membranes, and orthostatic hypotension.
- Educate patients about the importance of reporting any new or worsening symptoms.
- Be aware of potential drug interactions. Review the patient’s medication list for any potential conflicts.
Specific Lab Monitoring Schedule:
- Baseline: Serum creatinine, creatinine clearance, serum electrolytes (potassium, sodium, magnesium), complete blood count (CBC)
- During treatment (every 2-3 days): Serum creatinine, creatinine clearance, serum electrolytes
- As needed: Audiometry testing, additional electrolyte panels depending on patient response.
Remember, individualized patient management is key. Dosage adjustments and monitoring frequency should be tailored to the patient’s specific clinical condition and response to therapy.