Consult your doctor before taking Lasix while breastfeeding. This medication can pass into breast milk, and its potential impact on your baby needs careful assessment. Your physician will consider your individual circumstances and weigh the benefits of Lasix against any possible risks to your infant.
Factors influencing the decision include your specific medical condition requiring Lasix, your baby’s age and overall health, and the dosage of Lasix prescribed. Lower doses generally pose less risk, but close monitoring of your baby is still advised. Your doctor might recommend blood tests or close observation to check for any potential side effects in your baby.
Potential side effects in infants from Lasix exposure through breast milk may include dehydration and electrolyte imbalances. These can manifest as decreased urine output, lethargy, or unusual fussiness. Promptly report any such symptoms to your healthcare provider. Your doctor can offer guidance on managing potential complications and ensuring your baby’s well-being. Regular monitoring is key to safe medication management during breastfeeding.
Remember, this information is for guidance only and does not replace professional medical advice. Always discuss medication choices with your doctor or other qualified healthcare professional. They can provide tailored recommendations based on your individual needs and circumstances.
- Lasix While Breastfeeding: A Comprehensive Guide
- Understanding the Risks
- Alternatives and Considerations
- Communication is Key
- Disclaimer
- Understanding Lasix and its Mechanism
- Lasix and Milk Production: Potential Effects
- Lasix in Breast Milk: Transfer and Concentration
- Risks to the Infant: Potential Side Effects
- Alternatives to Lasix During Breastfeeding
- Dietary and Lifestyle Changes
- Other Medications
- Monitoring and Support
- When to Consult a Doctor: Necessary Precautions
- Monitoring Infant’s Health: Key Indicators
- Feeding and Hydration
- Vital Signs
- Other Indicators
- Key Observation Chart
- Seeking Medical Advice
- Weighing the Risks and Benefits: A Personalized Approach
- Assessing Your Situation
- Monitoring Your Baby
- Alternative Approaches
Lasix While Breastfeeding: A Comprehensive Guide
Avoid Lasix while breastfeeding unless explicitly directed by your doctor. The drug passes into breast milk, potentially affecting your baby.
Understanding the Risks
Lasix (furosemide) is a powerful diuretic. While it effectively removes excess fluid, it can also deplete essential electrolytes in both you and your baby. This can lead to dehydration, low potassium levels (hypokalemia), and other complications. Infants are particularly vulnerable to electrolyte imbalances.
- Dehydration: Lasix increases urine production, potentially dehydrating you and reducing your milk supply.
- Electrolyte Imbalances: Low potassium can cause muscle weakness, heart irregularities, and digestive problems in your baby.
- Other Potential Effects: While rare, other potential side effects in your baby might include jaundice or digestive upset.
Alternatives and Considerations
Discuss alternative treatments for your condition with your doctor. There may be medications or non-pharmaceutical approaches suitable for breastfeeding mothers.
- Alternative Medications: Your doctor may recommend a different diuretic with lower levels of excretion in breast milk, or an entirely different treatment approach.
- Dietary Changes: Adjusting your fluid and electrolyte intake can sometimes mitigate the need for strong diuretics.
- Non-Pharmacological Management: Depending on your condition, lifestyle modifications might prove helpful.
Communication is Key
Open communication with your physician is paramount. Discuss your breastfeeding status before starting any medication. Regularly monitor your baby for any unusual symptoms. Report any concerns immediately.
Disclaimer
This information is for educational purposes only and does not constitute medical advice. Always consult with your healthcare provider for personalized guidance regarding medication use during breastfeeding.
Understanding Lasix and its Mechanism
Lasix, or furosemide, acts as a potent loop diuretic. It works primarily in the loop of Henle, a section of your kidneys responsible for reabsorbing water and electrolytes. Lasix inhibits the sodium-potassium-chloride cotransporter (NKCC2) in this loop.
By blocking NKCC2, Lasix prevents your kidneys from reabsorbing sodium, chloride, and potassium. This leads to increased excretion of these substances in your urine, along with a significant increase in water excretion. This increased urine output is the primary mechanism by which Lasix lowers blood pressure and reduces fluid retention.
The magnitude of its effect on urine production directly influences its effectiveness in managing edema and hypertension. Importantly, potassium loss is a potential side effect due to its impact on potassium reabsorption. Doctors carefully monitor potassium levels during Lasix treatment.
Its effects are relatively rapid, with noticeable diuresis typically occurring within an hour of administration. Duration of action is usually between 6-8 hours, though this can vary depending on factors like dose and individual kidney function.
Remember to consult your healthcare provider for any questions or concerns regarding Lasix, especially if you’re breastfeeding.
Lasix and Milk Production: Potential Effects
Lasix (furosemide), a potent diuretic, can decrease milk production in breastfeeding mothers. This reduction happens because Lasix increases urine output, leading to dehydration. Dehydration directly impacts the body’s ability to produce breast milk.
The extent of milk reduction varies. Some mothers experience minimal changes, while others may notice a significant decrease in milk supply. Several factors influence the effect, including dosage, duration of Lasix use, and individual response.
- Dosage: Higher doses of Lasix generally lead to a more pronounced decrease in milk production than lower doses.
- Duration: Prolonged Lasix use might result in a more substantial reduction in milk supply compared to short-term use.
- Individual Variation: Each mother’s body responds differently to medication. Some are more sensitive to Lasix’s effects on milk production than others.
If you are prescribed Lasix while breastfeeding, discuss milk production concerns with your doctor or lactation consultant. They can help you weigh the risks and benefits of Lasix against potential impacts on breastfeeding. They may suggest strategies for minimizing the impact on your milk supply, such as increasing fluid intake.
- Hydration is key: Drink plenty of fluids to help maintain adequate milk production. This can partially offset the diuretic effects of Lasix.
- Frequent feeding: Regular nursing or pumping can help stimulate milk production and minimize supply reduction.
- Nutritional support: Maintaining a healthy diet rich in nutrients will help support your body’s ability to produce milk.
Closely monitor your baby’s weight and feeding patterns. If you notice any significant changes, consult your pediatrician. Remember, open communication with your healthcare providers is crucial for managing this situation safely and effectively.
Lasix in Breast Milk: Transfer and Concentration
Lasix (furosemide) does transfer into breast milk, but the amount is generally low. Studies show concentrations range from 0.1% to 10% of maternal serum levels. This means the baby receives a significantly smaller dose than the mother.
Several factors influence the concentration: maternal dose, time since administration, and the baby’s metabolism. Larger maternal doses result in higher concentrations in breast milk. Peak milk concentrations typically occur within 1-2 hours of maternal administration. Infant metabolism and renal function also play a role in how much furosemide the baby processes.
While generally considered safe, monitoring the infant for potential side effects like dehydration or electrolyte imbalances is important. These are rare but possible. Consult your doctor immediately if you observe any unusual symptoms in your baby.
Doctors often recommend careful weighing and monitoring of infant urine output, as well as regular electrolyte checks, particularly if higher Lasix doses are necessary. This helps ensure the baby’s hydration and electrolyte balance remain stable.
Remember to discuss this medication with your pediatrician or lactation consultant. They can provide tailored advice based on your specific situation and baby’s health.
Risks to the Infant: Potential Side Effects
Lasix (furosemide) passes into breast milk, so potential side effects in the nursing infant require careful consideration. While generally small amounts transfer, they can still impact the baby. Infants are particularly sensitive to medication side effects.
Common side effects may include dehydration and electrolyte imbalances. These can manifest as lethargy, poor feeding, and excessive thirst. Less frequently, infants might experience diarrhea. Severe dehydration can be dangerous; monitor your baby’s diaper output and overall hydration carefully.
| Side Effect | Symptoms | Action |
|---|---|---|
| Dehydration | Dry mouth, fewer wet diapers, sunken eyes, lethargy | Increase breastfeeding frequency, contact your doctor immediately. |
| Electrolyte Imbalance | Muscle weakness, vomiting, irritability, irregular heartbeat | Seek immediate medical attention. |
| Diarrhea | Frequent, watery stools | Monitor for dehydration; contact your doctor if concerned. |
Rare but serious complications can occur. These include low blood pressure and kidney problems. Prompt medical attention is necessary if you observe any signs of these conditions in your baby. Always inform your doctor that you are breastfeeding before starting any medication.
Regular monitoring of your infant’s weight and overall health is crucial during the period you are taking Lasix. Open communication with your pediatrician regarding your baby’s well-being is paramount. They can provide individualized advice and guidance, taking into account your baby’s unique needs and health status.
Alternatives to Lasix During Breastfeeding
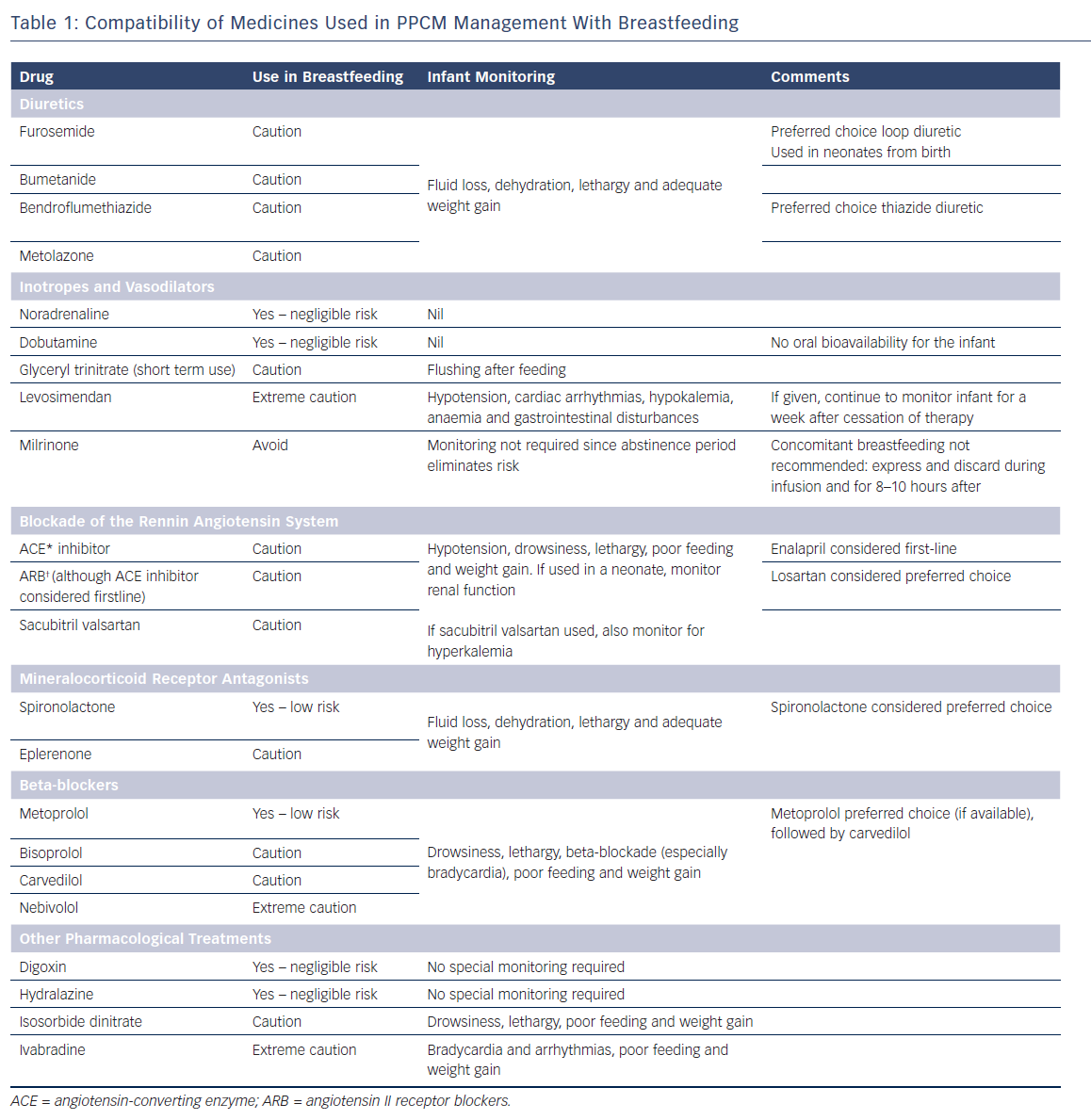
Your doctor might suggest alternative diuretics with a lower risk of transferring into breast milk. Spironolactone, for example, is often considered safer than Lasix during lactation. However, always discuss all medication options with your healthcare provider before making any changes to your treatment plan. They can assess your specific situation and recommend the best course of action.
Dietary and Lifestyle Changes
Before considering medication, explore non-pharmaceutical approaches to manage fluid retention. Increasing your potassium intake through foods like bananas, potatoes, and spinach can help balance electrolyte levels often affected by diuretics. Reducing sodium in your diet significantly impacts fluid retention. Drink plenty of water; it sounds counterintuitive, but adequate hydration can actually help your body flush out excess fluid more effectively. Regular, moderate exercise also supports fluid balance.
Other Medications
Depending on the underlying condition necessitating Lasix, other medications might be more appropriate while breastfeeding. Your physician may prescribe different treatments to address the root cause of your fluid retention. This personalized approach minimizes the need for medications that could potentially harm your baby.
Monitoring and Support
Regularly check in with your doctor for monitoring. They can evaluate your condition, adjust your treatment, and offer support. Don’t hesitate to communicate any concerns regarding breastfeeding or medication side effects. Working closely with your healthcare provider ensures your and your baby’s well-being.
When to Consult a Doctor: Necessary Precautions
Contact your doctor immediately if your baby shows signs of dehydration, such as decreased urination, dry mouth, or sunken eyes. These symptoms may indicate Lasix is impacting your baby negatively.
Report any unusual changes in your baby’s feeding patterns or weight gain. Significant weight loss or reduced appetite warrants medical attention.
Discuss any potential drug interactions with your physician before starting Lasix, especially if you are taking other medications. Your doctor can help assess potential risks.
Monitor your baby’s electrolyte levels regularly as directed by your doctor. Lasix can affect potassium levels, requiring close monitoring.
If you experience any adverse effects while taking Lasix, such as dizziness, weakness, or muscle cramps, consult your healthcare provider promptly. Your health is paramount.
Regular check-ups with your pediatrician are strongly recommended during the duration of your Lasix treatment to ensure your baby’s well-being.
Remember to always inform your doctor about your breastfeeding status before starting any new medication, including Lasix.
Discontinue Lasix immediately if you suspect an allergic reaction. Symptoms may include rash, itching, swelling, or difficulty breathing.
Always prioritize open communication with your doctor. They can provide personalized advice and guidance tailored to your situation.
Monitoring Infant’s Health: Key Indicators
Closely watch your baby’s weight and urination. Weight gain should be consistent. Monitor diaper changes; fewer wet diapers might suggest dehydration. Contact your pediatrician immediately if you see significant changes.
Feeding and Hydration
Track feeding frequency and volume. Note any changes in appetite or sucking ability. Dehydration symptoms include sunken fontanelles (soft spots on the head), dry mouth, and decreased tear production. Report these immediately.
Vital Signs
Regularly check your baby’s temperature. A fever can indicate infection. Monitor heart rate and breathing; rapid breathing or a very slow heart rate require immediate attention. Use a digital thermometer for accurate readings.
Other Indicators
Observe your baby’s skin for jaundice (yellowing). Note any unusual lethargy, irritability, or changes in activity level. Pay attention to stool consistency and frequency; alterations can point to complications.
Key Observation Chart
| Indicator | Normal Range/Expectation | Concerning Sign | Action |
|---|---|---|---|
| Weight Gain | Consistent weekly increase | Significant weight loss | Contact pediatrician immediately |
| Wet Diapers | 6-8 per day (adjust for age) | Fewer than 4 per day | Contact pediatrician immediately |
| Feeding | Regular, consistent feeding | Poor feeding, refusal to feed | Contact pediatrician |
| Temperature | 97.9-99.5°F (36.6-37.5°C) | Temperature above 100.4°F (38°C) | Contact pediatrician immediately |
| Skin | Normal color and turgor | Jaundice, pallor, rash | Contact pediatrician |
Seeking Medical Advice
Don’t hesitate to call your pediatrician for any concerns. Early detection is crucial for optimal infant health.
Weighing the Risks and Benefits: A Personalized Approach
Consult your doctor immediately. They will assess your individual needs and health status, considering factors like the severity of your condition requiring Lasix, your baby’s age and health, and your milk production. This personalized assessment is paramount.
Assessing Your Situation
Your doctor will discuss the potential benefits of Lasix for you against the potential risks to your baby. Lasix can pass into breast milk in small amounts. For some infants, this might not cause any problems. However, others may experience electrolyte imbalances or dehydration, necessitating close monitoring. Your doctor can help you determine if the benefits outweigh the risks in your unique case.
Monitoring Your Baby
If you choose to use Lasix while breastfeeding, closely monitor your baby for any signs of dehydration, such as fewer wet diapers, lethargy, or sunken eyes. Regular weigh-ins are also vital. Report any concerns to your doctor promptly. They might suggest alternative medications or breastfeeding strategies if needed.
Alternative Approaches
Your doctor might explore alternative treatments for your condition that don’t involve Lasix or that pose a lower risk to your baby. They may also advise on techniques to minimize the amount of medication reaching your breast milk, including adjusting the timing of medication intake.
Remember: Open communication with your healthcare provider is key to making the best decision for you and your baby.