If you’re considering Clomid and have a blood clotting disorder, consult your doctor immediately. This isn’t a decision you should make alone. Open communication with your healthcare provider is paramount.
Clomid, or clomiphene citrate, can increase the risk of blood clots in some individuals. This risk is amplified if you already have a pre-existing clotting disorder such as Factor V Leiden, antiphospholipid syndrome, or a history of venous thromboembolism (VTE). Your physician needs to weigh the potential benefits of Clomid against these increased risks, tailoring a plan specifically for your situation.
Specific blood tests may be necessary to assess your individual risk profile. These tests could include clotting factor assays or other specialized analyses. Depending on the results, alternative fertility treatments may be explored. Remember, your doctor will guide you through the options available, based on your unique health profile.
Never self-medicate or adjust your dosage without explicit instruction from your physician. Close monitoring of your blood clotting parameters might be needed during Clomid therapy. Report any unusual symptoms, such as leg pain, swelling, shortness of breath, or chest pain, without delay.
- Taking Clomid and Blood Clotting Disorders
- Clomid’s Mechanism of Action and Potential Blood Clotting Impacts
- Identifying Individuals at Risk for Blood Clots While on Clomid
- Factors Increasing Your Risk
- Specific Medications and Interactions
- Monitoring and Prevention
- Age and Pregnancy
- Specific Blood Clotting Disorders Exacerbated by Clomid
- Factor V Leiden
- Antiphospholipid Syndrome (APS)
- Inherited Thrombophilias
- Symptoms of Blood Clots to Watch For During Clomid Treatment
- Diagnostic Tests to Monitor for Blood Clot Formation
- Preventive Measures and Lifestyle Modifications to Reduce Risk
- Managing Underlying Conditions
- Medication and Monitoring
- Supplements
- Stress Management
- Management Strategies for Blood Clots During Clomid Therapy
- Diagnostic Testing and Confirmation
- Treatment Approaches
- Monitoring and Follow-up
- Preventing Future Clots
- Important Note:
- Seeking Medical Advice and Ongoing Monitoring
Taking Clomid and Blood Clotting Disorders
Consult your doctor before starting Clomid if you have a blood clotting disorder. Clomid can increase the risk of blood clots in some women. Your doctor will assess your individual risk factors and determine if Clomid is safe for you.
Specific blood clotting disorders like Factor V Leiden or antiphospholipid syndrome significantly raise your risk of complications with Clomid. Open communication with your physician is paramount; discuss your complete medical history, including family history of clotting disorders.
Regular monitoring may be necessary during Clomid treatment. This could involve blood tests to track clotting factors and check for any signs of thrombosis. Your doctor will guide you on the appropriate frequency and type of monitoring.
Should you experience symptoms like sudden leg pain, shortness of breath, chest pain, or severe headaches during Clomid use, seek immediate medical attention. These could be indicators of a blood clot.
Alternative fertility treatments may be considered if Clomid is deemed too risky given your blood clotting disorder. Your doctor will discuss these options, tailoring the approach to your specific circumstances.
Remember, proactive communication with your healthcare provider is key to managing your fertility journey safely and effectively. Don’t hesitate to ask questions and voice your concerns.
Clomid’s Mechanism of Action and Potential Blood Clotting Impacts
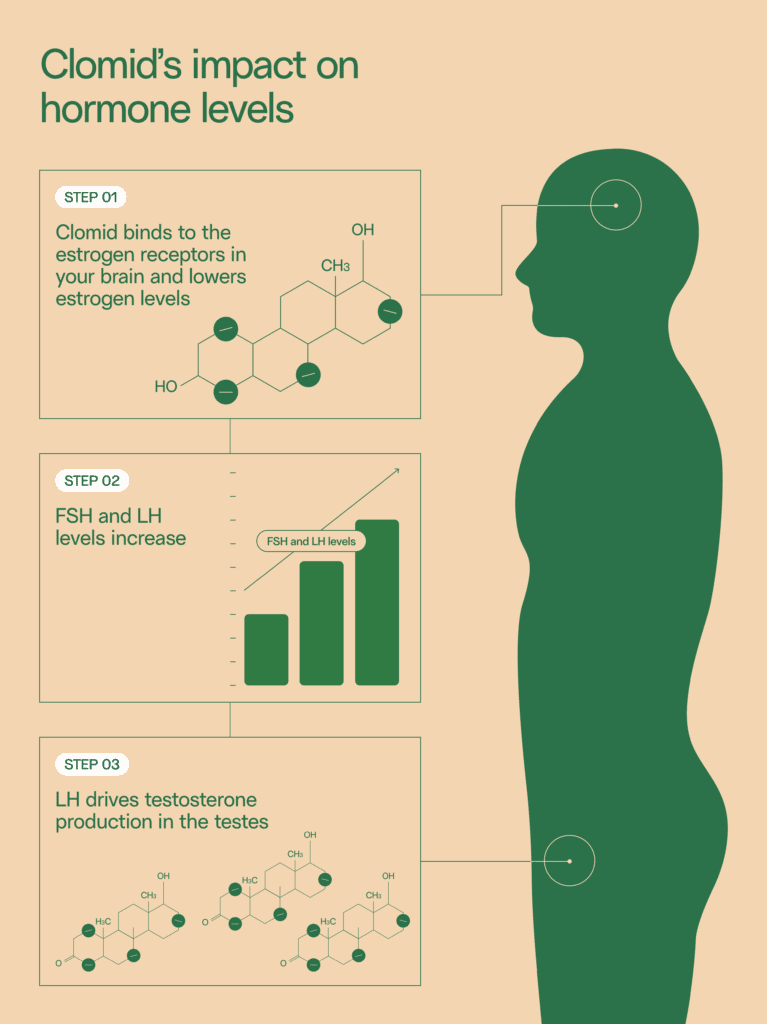
Clomid, or clomiphene citrate, stimulates ovulation by blocking estrogen receptors in the hypothalamus and pituitary gland. This blockage increases the production of gonadotropin-releasing hormone (GnRH), leading to a surge in follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Higher FSH levels promote follicle growth, while the LH surge triggers ovulation.
Concerning blood clotting, Clomid’s impact is indirect and not fully understood. Some studies suggest a potential association between Clomid use and an increased risk of thromboembolic events, such as deep vein thrombosis (DVT) and pulmonary embolism (PE). This increased risk appears to be small, yet individuals with pre-existing clotting disorders or risk factors should carefully discuss this potential complication with their healthcare provider before initiating Clomid therapy. Regular monitoring for symptoms of clotting problems, including leg pain, swelling, shortness of breath, and chest pain, is recommended for patients taking Clomid.
The mechanism behind this potential link isn’t definitively established. It’s hypothesized that Clomid may influence clotting factors through its effects on estrogen levels or by other, yet unidentified, pathways. Further research is needed to fully elucidate these interactions.
Caution: This information is for educational purposes only and does not constitute medical advice. Always consult your physician before starting any medication, especially if you have a history of blood clotting disorders or risk factors. They can assess your individual risk and provide personalized recommendations.
Remember: Open communication with your doctor is key to managing any potential risks associated with Clomid use.
Identifying Individuals at Risk for Blood Clots While on Clomid
Pre-existing conditions significantly increase your risk. If you have a personal or family history of blood clots (thrombosis), a clotting disorder like Factor V Leiden, or conditions like antiphospholipid syndrome, discuss Clomid use with your doctor. These conditions make you considerably more susceptible to blood clot formation.
Factors Increasing Your Risk
Certain lifestyle choices influence your risk profile. Smoking heavily increases your risk of blood clots, independent of Clomid use. Similarly, prolonged immobility, such as long flights or bed rest, can elevate your risk. Obesity also increases the chance of blood clot development. Consider adopting healthier habits, like quitting smoking and maintaining a healthy weight, before and during Clomid treatment.
Specific Medications and Interactions
Some medications increase the risk of blood clots. Talk to your doctor about any other medications you are taking, including hormonal birth control pills and certain hormone replacement therapies. They can assess potential drug interactions and advise you appropriately. Always inform your doctor about all your medications and supplements.
Monitoring and Prevention
Regular monitoring is vital. Your physician may recommend blood tests to assess your clotting factors before, during, and after Clomid treatment. They may also prescribe blood thinners in certain high-risk situations. Proactive monitoring and open communication with your doctor are your best defenses.
Age and Pregnancy
Age plays a role. Older individuals generally have a higher risk of blood clots. Pregnancy significantly increases the risk of blood clots, and Clomid itself is used to increase the chance of pregnancy. Open communication with your doctor about your age and plans for pregnancy is therefore paramount.
Specific Blood Clotting Disorders Exacerbated by Clomid
Clomid, while effective for inducing ovulation, can increase the risk of thromboembolic events in women with certain blood clotting disorders. This heightened risk stems from Clomid’s impact on factors influencing blood coagulation. Therefore, careful consideration is necessary before prescribing Clomid to patients with a history of clotting problems.
Factor V Leiden
Women with Factor V Leiden, a common inherited clotting disorder, face a significantly elevated risk of deep vein thrombosis (DVT) and pulmonary embolism (PE) when taking Clomid. The combination increases the likelihood of abnormal blood clot formation. Consult your doctor immediately if you have Factor V Leiden and are considering Clomid. Thorough risk assessment and possibly alternative treatment options should be discussed.
Antiphospholipid Syndrome (APS)
Patients with APS, an autoimmune disorder affecting blood clotting, are also at increased risk of thrombosis while using Clomid. APS already disrupts the body’s natural anticoagulant mechanisms; Clomid may further exacerbate this imbalance. Regular monitoring, including blood tests, is crucial during Clomid treatment for individuals with APS. Close collaboration with a hematologist is highly recommended.
Inherited Thrombophilias
Other inherited thrombophilias, such as deficiencies in Protein S or Protein C, can interact negatively with Clomid, raising the risk of blood clots. These conditions impair the body’s ability to break down clots, making Clomid use potentially hazardous. Always disclose your family history and any known clotting disorders to your healthcare provider before starting Clomid.
Symptoms of Blood Clots to Watch For During Clomid Treatment
If you’re taking Clomid and experience any of the following, seek immediate medical attention. These symptoms could indicate a blood clot, a serious complication that requires prompt treatment.
- Chest pain: Sharp, stabbing pain, possibly radiating to your arm or jaw. This is a classic sign of a pulmonary embolism (blood clot in the lung).
- Shortness of breath: Sudden difficulty breathing, even at rest. This can accompany chest pain but may occur independently.
- Leg pain or swelling: Pain, tenderness, or swelling in one leg, often accompanied by redness or warmth. This suggests a deep vein thrombosis (DVT), a blood clot in a leg vein.
- Coughing up blood: This is a serious symptom and warrants immediate medical help.
- Sudden dizziness or fainting: These can be signs of a blood clot affecting the brain.
- Rapid heart rate: An unexpectedly elevated heart rate, even without exertion.
- Sudden severe headache: A headache significantly different from your usual headaches.
This list is not exhaustive, and other symptoms are possible. Remember, early detection and treatment of blood clots are key to preventing serious complications. Don’t hesitate to contact your doctor if you have any concerns.
- Keep a detailed record of your symptoms: Note the time of onset, severity, and any associated factors.
- Communicate clearly with your doctor: Provide all relevant information about your symptoms and medication.
- Follow your doctor’s instructions carefully: Adhere to prescribed medication and follow-up appointments.
Your health is paramount. Prompt action can significantly improve outcomes.
Diagnostic Tests to Monitor for Blood Clot Formation
Your doctor might order several tests to assess your risk of blood clots while taking Clomid. A complete blood count (CBC) measures various blood components, including platelets, which play a key role in clotting. Low platelet counts can increase clot risk.
A prothrombin time (PT) and partial thromboplastin time (PTT) test evaluate how quickly your blood clots. Abnormal results suggest potential clotting disorders. These tests are vital for identifying deficiencies in clotting factors.
D-dimer testing measures fibrin degradation products, byproducts of clot breakdown. Elevated levels may indicate the presence of a blood clot, though this test isn’t conclusive on its own and needs further investigation.
Ultrasound, particularly a Doppler ultrasound, can visualize blood vessels and identify potential clots. This imaging technique offers a direct look at veins and arteries, revealing obstructions if present. This method is frequently used to investigate suspected deep vein thrombosis (DVT).
Genetic testing may be considered to identify inherited clotting disorders. This approach helps assess long-term risk and provides insight into your predisposition for developing clotting issues.
Regular monitoring with these tests allows your healthcare provider to adjust your treatment or take appropriate preventative measures as needed. Open communication with your doctor regarding any symptoms, like pain, swelling, or redness in your legs, is paramount for timely diagnosis and intervention.
Preventive Measures and Lifestyle Modifications to Reduce Risk
Maintain a healthy weight. Excess weight increases clotting risk. Aim for a BMI within the healthy range.
Regularly exercise. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. This improves circulation and reduces clotting factors.
Prioritize a balanced diet rich in fruits, vegetables, and whole grains. Limit saturated and trans fats, processed foods, and excessive sugar intake. These dietary changes contribute to overall vascular health.
Hydrate consistently. Drink plenty of water throughout the day to maintain healthy blood viscosity.
Managing Underlying Conditions
Carefully manage any existing health conditions, such as diabetes or high blood pressure, that could increase clotting risk. Work closely with your doctor to maintain optimal control of these conditions.
Medication and Monitoring
Strictly follow your doctor’s instructions for Clomid and any other medications. Attend all scheduled blood tests and appointments for careful monitoring of your blood clotting factors.
Discuss any concerns or side effects immediately with your healthcare provider. Prompt reporting is key to managing potential complications.
Avoid smoking. Smoking significantly elevates the risk of blood clots. Quitting smoking offers immediate health benefits.
Supplements
Consult your doctor before taking any supplements, especially those affecting blood clotting, such as vitamin K or fish oil. They can advise on appropriate dosages and potential interactions.
Stress Management
Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises. Chronic stress can influence clotting factors.
Management Strategies for Blood Clots During Clomid Therapy
If you experience symptoms suggesting a blood clot while taking Clomid (such as chest pain, shortness of breath, or leg swelling), seek immediate medical attention. This is paramount.
Diagnostic Testing and Confirmation
Your doctor will likely order blood tests to check for clotting factors and imaging studies like ultrasound or CT scans to locate and assess the clot. A D-dimer test might be used to rule out a clot, but a positive result doesn’t definitively confirm one. Further testing is often necessary.
Treatment Approaches
- Anticoagulation Therapy: This is a cornerstone of treatment. Your doctor may prescribe blood thinners like heparin (often given intravenously initially) or warfarin (oral medication requiring regular blood monitoring). The choice depends on the type and location of the clot, your overall health, and other medications you are taking. Direct acting oral anticoagulants (DOACs) like apixaban or rivaroxaban are also possibilities.
- Compression Therapy: For clots in the legs (deep vein thrombosis or DVT), compression stockings can help reduce swelling and improve blood flow. Your doctor will provide guidance on proper usage.
- Lifestyle Modifications: Staying well-hydrated is crucial. Regular, gentle movement, as advised by your healthcare provider, is recommended to aid circulation, but avoid strenuous activity. Smoking cessation is vital as it increases clotting risk.
- Clomid Discontinuation: In many cases, Clomid will be discontinued while the clot is treated. Your doctor will assess the risk/benefit ratio and make a determination based on your individual circumstances and response to treatment. Alternatives to Clomid for fertility treatment may be discussed.
Monitoring and Follow-up
Regular monitoring of your blood clotting parameters is crucial during and after treatment. Follow-up appointments allow your doctor to assess your progress, adjust medication as needed, and identify any potential complications.
Preventing Future Clots
- Maintain a healthy weight.
- Manage any underlying medical conditions that increase clotting risk, such as inherited thrombophilias.
- Discuss all medications and supplements with your doctor before starting them.
Important Note:
This information is for general knowledge and does not replace professional medical advice. Always consult your doctor or healthcare provider for personalized guidance and treatment.
Seeking Medical Advice and Ongoing Monitoring
Consult your doctor immediately if you experience any unusual symptoms, such as severe headaches, chest pain, shortness of breath, or leg swelling. These could indicate a potential blood clot.
Regular blood tests are necessary to monitor your clotting factors while taking Clomid. Your doctor will schedule these tests based on your individual needs and risk factors. Follow their recommendations meticulously.
Open and honest communication with your healthcare provider is paramount. Report any changes in your health status, including medication side effects and lifestyle changes. This allows for proactive management of potential risks.
Maintain a detailed record of your Clomid dosage, blood test results, and any symptoms you experience. This record helps you and your doctor track your progress and identify potential problems early.
| Symptom | Action |
|---|---|
| Severe headache | Contact your doctor immediately |
| Chest pain | Seek immediate medical attention |
| Shortness of breath | Go to the emergency room |
| Leg swelling | Contact your doctor promptly |
Discuss alternative therapies or modifications to your treatment plan with your doctor if concerns arise. They can help assess your risk and adjust your care accordingly. Remember that proactive monitoring and open communication are key to safe and effective treatment.