Reactive arthritis often subsides within a year for many individuals. However, a significant portion experience persistent symptoms, sometimes requiring long-term management. This isn’t a one-size-fits-all situation; recovery varies depending on several factors.
Factors influencing recovery include the severity of the initial infection triggering the arthritis, your overall health, and how promptly you receive treatment. Early diagnosis and aggressive management significantly improve your chances of a faster and more complete recovery. This means acting quickly when you notice symptoms like joint pain, swelling, and skin rashes.
Treatment plans typically involve a combination of approaches. These may include medication to reduce inflammation and pain, physical therapy to maintain joint mobility and strengthen muscles, and lifestyle modifications such as diet changes and regular exercise. Consistent adherence to your doctor’s recommended treatment plan is key. Your rheumatologist will personalize your care based on your specific needs and condition.
While complete remission is possible for many, some individuals may experience flare-ups throughout their lives. Regular check-ups with your physician are vital for monitoring your condition and adjusting your treatment as needed. Proactive management empowers you to minimize long-term complications and maintain a higher quality of life.
- Does Reactive Arthritis Go Away?
- Understanding Reactive Arthritis’s Progression
- The Acute Phase
- The Chronic Phase
- Factors Influencing Progression
- Long-Term Outlook
- Managing the Disease
- The Role of Treatment in Long-Term Outcomes
- Factors Influencing Recovery Time
- Individual Factors
- Treatment Adherence
- Lifestyle Choices
- Comorbidities
- Severity of Initial Infection
- Living with Reactive Arthritis: Managing Symptoms
- Medication Management
- Self-Care Strategies
- Lifestyle Adjustments
- Seeking Support
- Regular Monitoring
- When to Seek Further Medical Attention
- Concerning Symptoms Requiring Urgent Care
- Potential for Long-Term Complications and Remission
- Understanding Remission
- Potential Long-Term Complications
- Managing Long-Term Risks
- Prognosis
Does Reactive Arthritis Go Away?
Reactive arthritis often resolves within a year for most people. However, some individuals experience persistent symptoms or recurring episodes. Successful treatment depends heavily on prompt diagnosis and adherence to the prescribed plan.
Here’s what you should know:
- Symptom Management: Your doctor will likely prescribe medication to manage pain, inflammation, and other symptoms. This might include NSAIDs (nonsteroidal anti-inflammatory drugs) or other medications.
- Lifestyle Changes: Maintaining a healthy lifestyle can significantly impact your recovery. This includes a balanced diet, regular low-impact exercise, and sufficient rest. Avoid activities that aggravate your joints.
- Physical Therapy: A physical therapist can create a personalized exercise program to strengthen muscles, improve range of motion, and reduce joint stiffness. This plays a critical role in long-term recovery.
- Long-term Outlook: While many individuals experience remission, some develop chronic reactive arthritis. Regular follow-up appointments with your doctor are crucial for monitoring your condition and adapting treatment as needed.
Factors influencing recovery time include:
- Severity of the initial infection: A more severe initial infection might lead to more prolonged symptoms.
- Promptness of treatment: Early intervention is often associated with better outcomes.
- Individual response to treatment: Each person responds differently to medication and therapies.
- Overall health and genetics: Pre-existing health conditions and genetic predispositions can affect recovery.
If you suspect you have reactive arthritis, seek medical attention immediately. Early diagnosis and treatment are key to achieving the best possible outcome. Remember, consistent communication with your healthcare provider is vital throughout the recovery process.
Understanding Reactive Arthritis’s Progression
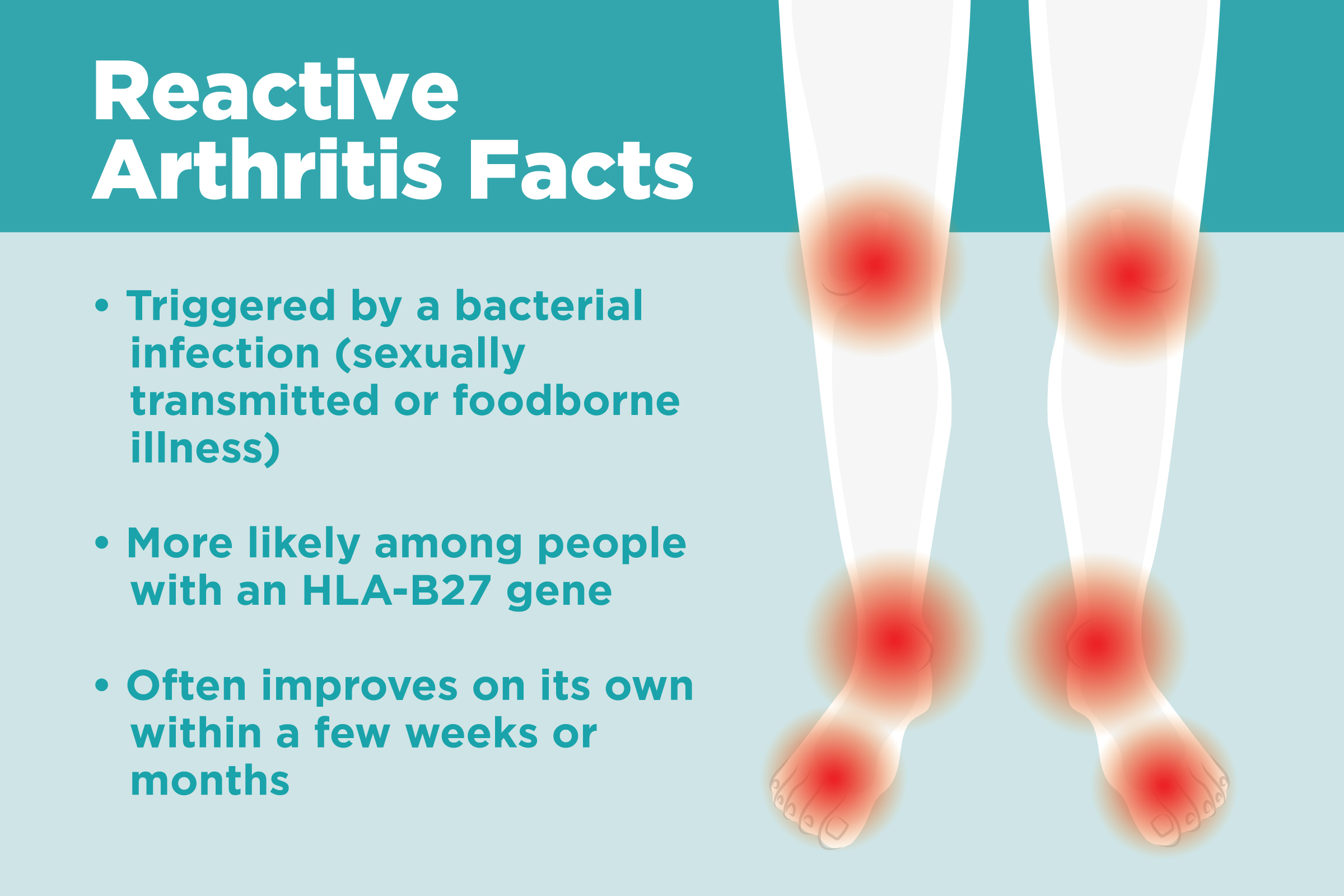
Reactive arthritis usually follows an infection, typically gastrointestinal or urinary tract. Symptoms generally appear within 1-4 weeks after the initial infection. The severity varies greatly among individuals.
The Acute Phase
This initial phase is characterized by intense joint pain, swelling, and stiffness, often affecting the lower extremities like knees and ankles. Eye inflammation (uveitis) and skin rashes are also common during this phase. This period often lasts several weeks, with symptoms gradually decreasing in intensity over several months.
The Chronic Phase
Some individuals transition into a chronic phase. This means joint inflammation and pain persist, though usually at a lower intensity than the acute phase. This chronic inflammation may cause ongoing joint damage over time. For some, the disease may become relatively inactive, with only occasional flares of symptoms. Regular monitoring and appropriate management are crucial during this phase.
Factors Influencing Progression
Several factors influence how reactive arthritis progresses. Genetic predisposition plays a role, as does the type and severity of the initial infection. Prompt diagnosis and early treatment can significantly impact long-term outcomes. Lifestyle choices, such as maintaining a healthy weight and engaging in regular, low-impact exercise, are beneficial. Ignoring symptoms could result in persistent joint damage.
Long-Term Outlook
Many individuals experience significant improvement, with symptoms resolving within a year. However, some may experience persistent joint problems. The disease’s trajectory is highly individual. Regular consultations with a rheumatologist allow for tailored management, aimed at minimizing long-term complications and maximizing quality of life.
Managing the Disease
Treatment focuses on managing pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first line of treatment. In more severe cases, other medications, such as corticosteroids or disease-modifying antirheumatic drugs (DMARDs), may be necessary. Physical therapy and occupational therapy can also help maintain joint function and improve daily living skills.
The Role of Treatment in Long-Term Outcomes
Early and aggressive treatment significantly improves long-term outcomes for reactive arthritis. This means promptly addressing symptoms and underlying infections.
Nonsteroidal anti-inflammatory drugs (NSAIDs) effectively manage pain and inflammation. Physical therapy plays a crucial role, improving joint mobility and function, preventing long-term stiffness.
For persistent inflammation, doctors may prescribe disease-modifying antirheumatic drugs (DMARDs), such as sulfasalazine or methotrexate. These medications alter the disease’s course, reducing joint damage. In some cases, biologics, targeted therapies that affect specific parts of the immune system, provide additional benefit.
Regular follow-up appointments are key. Consistent monitoring allows doctors to adjust treatment plans as needed, optimizing results and mitigating potential complications. Patients should actively participate in their care, reporting any changes in symptoms and adhering to prescribed treatment plans.
Lifestyle modifications support treatment. Maintaining a healthy weight reduces stress on affected joints. Regular exercise, tailored to individual capabilities, improves strength and flexibility. A balanced diet provides necessary nutrients for tissue repair.
Successful long-term management often involves a multidisciplinary approach. This includes rheumatologists, physical therapists, and possibly other specialists. This collaborative care model ensures comprehensive and individualized treatment.
Factors Influencing Recovery Time
Early diagnosis significantly impacts recovery. Prompt treatment with antibiotics for the initial infection speeds healing and minimizes joint damage. A delay can lead to prolonged symptoms.
Individual Factors
Your immune system plays a key role. A strong immune response might lead to faster resolution, while a weakened system may prolong the condition. Genetic predisposition also influences how your body reacts to the inflammation. Certain genetic markers are associated with more severe or persistent symptoms.
Treatment Adherence
Consistent medication use, prescribed by your doctor, is crucial. Following the prescribed course of antibiotics and other medications, such as NSAIDs or biologics, is paramount for effective management. Physical therapy, when recommended, should be undertaken diligently.
Lifestyle Choices
Maintaining a healthy lifestyle aids recovery. A balanced diet rich in anti-inflammatory foods supports your body’s natural healing process. Regular, moderate exercise strengthens muscles and improves joint mobility, helping reduce stiffness and pain. Sufficient rest allows your body to repair and rebuild.
Comorbidities
Pre-existing conditions, particularly autoimmune diseases, can complicate recovery and increase the duration of symptoms. Managing these conditions effectively can minimize their impact on reactive arthritis. Close communication with your physician regarding all health issues is vital.
Severity of Initial Infection
The initial infection’s severity directly affects the subsequent inflammatory response. A more severe infection tends to result in more pronounced and prolonged reactive arthritis symptoms.
Living with Reactive Arthritis: Managing Symptoms
Prioritize regular exercise. Low-impact activities like swimming or cycling help maintain mobility and reduce stiffness. Aim for at least 30 minutes most days of the week. Listen to your body and rest when needed.
Manage your diet. A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can significantly improve symptoms. Reduce processed foods, sugar, and saturated fats. Consult a registered dietitian for personalized dietary advice.
Medication Management
Work closely with your rheumatologist to find the right medication regimen. This may include NSAIDs for pain relief, disease-modifying antirheumatic drugs (DMARDs) to slow disease progression, or biologics for severe cases. Strictly follow your doctor’s instructions and report any side effects immediately.
Self-Care Strategies
Apply heat or cold packs to inflamed joints for pain relief. Heat can help relax muscles, while cold can reduce swelling. Experiment to find what works best for you. Gentle stretching and range-of-motion exercises can also help maintain joint flexibility.
| Symptom | Management Strategy |
|---|---|
| Joint Pain | Rest, ice/heat, NSAIDs, physical therapy |
| Fatigue | Prioritize sleep, manage stress, pace activities |
| Eye Inflammation | Eye drops prescribed by ophthalmologist |
| Skin Rash | Keep skin clean and dry, avoid irritants |
Lifestyle Adjustments
Prioritize sleep. Aim for 7-9 hours of quality sleep each night. Stress management techniques, such as meditation or yoga, can significantly reduce pain and inflammation. Learn to pace yourself throughout the day, avoiding overexertion.
Seeking Support
Connect with support groups for people with reactive arthritis. Sharing experiences and coping strategies with others facing similar challenges can be invaluable. Consider seeking counseling or therapy to help manage the emotional aspects of living with a chronic illness.
Regular Monitoring
Schedule regular check-ups with your rheumatologist to monitor disease activity and adjust treatment as needed. Early detection of flares and proactive management can minimize long-term complications.
When to Seek Further Medical Attention
Contact your doctor immediately if you experience new or worsening symptoms. This includes persistent fever above 101°F (38.3°C), significant joint pain limiting your daily activities, eye redness or pain (iritis), or difficulty breathing.
Concerning Symptoms Requiring Urgent Care
Seek immediate medical attention if you notice signs of infection, such as pus around a joint, increasing skin redness or warmth around a joint, or severe fatigue alongside these symptoms. These could indicate a serious complication requiring prompt treatment with antibiotics or other interventions. Don’t delay; rapid action is vital in these cases.
If your symptoms don’t improve or worsen despite treatment, schedule a follow-up appointment with your rheumatologist or doctor. They can adjust your treatment plan as needed or refer you to specialists for additional support. Regular monitoring helps ensure optimal management of your condition.
Potential for Long-Term Complications and Remission
Reactive arthritis can remit, meaning symptoms subside significantly or completely. However, long-term complications are possible, and proactive management is key.
Understanding Remission
Complete remission is when all symptoms disappear. Partial remission involves a significant reduction in symptom severity, allowing for a better quality of life. The timeline for remission varies greatly; some experience it within months, while others may have persistent symptoms for years. Factors influencing remission duration include the triggering infection’s severity, prompt treatment, and individual immune response.
- Early and aggressive treatment improves the likelihood of quicker and more complete remission.
- Lifestyle changes such as regular exercise (if tolerated), a balanced diet, and stress management techniques can positively impact the course of the disease and improve overall well-being.
- Close monitoring by your rheumatologist is vital. Regular check-ups allow for early detection of complications and adjustments to your treatment plan.
Potential Long-Term Complications
Although many individuals achieve remission, persistent or recurring symptoms are possible. These can include:
- Chronic joint pain and inflammation leading to stiffness and limited range of motion.
- Eye inflammation (uveitis), potentially causing vision problems if left untreated.
- Skin lesions, including psoriasis or keratoderma blennorrhagicum.
- Urethritis or cervicitis (inflammation of the urethra or cervix).
- Aortitis (inflammation of the aorta) – a less common but potentially serious complication.
Managing Long-Term Risks
Regular consultations with your healthcare team and adherence to prescribed treatment plans are crucial for minimizing the risk of long-term complications. This often involves medications to manage inflammation and pain, as well as physical therapy to improve joint function and mobility. Open communication with your doctor is paramount; don’t hesitate to express any concerns or changes in your symptoms.
Prognosis
While reactive arthritis can present challenges, many individuals achieve long-term remission with appropriate care. The likelihood of a favorable outcome is significantly enhanced by early diagnosis, prompt treatment, and consistent follow-up with your healthcare provider. A proactive approach to managing the condition can greatly improve your long-term outlook.